Abstract
Diffuse large b-cell lymphoma (DLBCL) with CNS relapse or progression has a poor prognosis. Prior studies noted certain factors which increased the risk of CNS relapse: bone marrow involvement, type as well as number (1+) of extra-nodal sites, age over 60, and increasing International Prognostic Index (IPI) score. However, these were prior to the advent of rituximab (R), which has been suggested to lower CNS relapse when used in combination with CHOP therapy. To our knowledge, no one has looked at the incidence of CNS relapse with regards to extranodal disease in the rituximab era.
Retrospective chart review of patients with DLBCL treated with multiagent induction therapy including rituximab from July‘08 to Jan’12 at Moffitt Cancer Center. Age, stage, IPI score, extra-nodal site, number of nodal sites, and use of intrathecal prophylaxis (IT), were evaluated for their impact on the risk of developing CNS relapse. For those who had complete response to initial therapy, time to progression(TTP) for CNS relapse was measured from completion date of first set of chemo cycles to date of CNS relapse (those who did not CNS relapse were censored at last follow up). TTP was censored at 6 years. Progression free survival(PFS) was measured from date of diagnosis to date of CNS or systemic relapse or death (those who were alive without relapse were censored at last follow up). Overall survival (OS) was measure from date of diagnosis to date of death. Stratified Kaplan Meier curves(with log rank p-values) and Cox PH models(with Wald p-values) were used to explore potential risk factors associated with relapse.
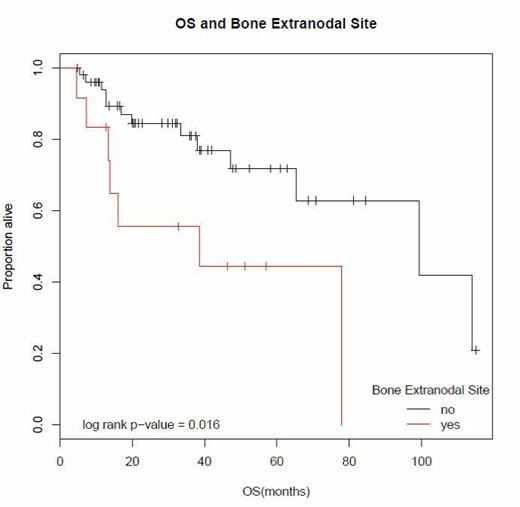
Sixty-four patients with DLBCL who received induction therapy were evaluated: median age (range) = 65 (24-93) years; male =56%; IPI scores at diagnosis: 1 (43.8%), 2(21.9%), 3(15.6%); median length of follow up from time of diagnosis = 32 months. All the patients received a regimen containing rituximab, and 92% of patients received R-Chop as treatment. IT prophylaxis with methotrexate was used in 28% of the patients. Incidence of CNS relapse in our study population= 17.3% (n=9) The risk of CNS relapse varied depending on the extranodal site. Those with bone marrow and/or musculoskeletal involvement had an increased risk, with 78% of the CNS relapses occurring in patients with one or both of these sites of involvement. The hazard ratio (HR) for CNS relapse for patients with bone marrow and musculoskeletal involvement was 2.53 and 2.74, respectively (p=0.20 and p=0.13). Other extranodal sites of disease such as visceral organs, genital urinary tract, nasopharynx, or skin did not seem to significantly contribute to the risk of CNS relapse. Patients with bone marrow involvement also had an inferior overall survival (HR=3.05, Wald p=0.02) (see figure 1). Though not statistically significant (log rank p=0.126), those receiving IT methotrexate prophylaxis appear to have longer PFS than those who did not, with 83% alive without relapse at 6 years compared to 43% (see figure 2).
Overall survival curve in patients with DLBCL and bone marrow involvement.
Despite the addition of rituximab to multiagent chemotherapy, those with bone marrow and musculoskeletal involvement still had a significantly higher risk of CNS relapse. There is a trend which suggests intrathecal prophylaxis with methotrexate can improve progression free survival and is still possibly beneficial in high risk DLBCL patients even in the rituximab era. Larger prospective studies are needed to determine the true benefit of prophylactic IT therapy in this population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal