Abstract
Histologic transformation of low grade non Hodgkin lymphoma (LG-NHL) occurs with a variable frequency. Several factors have been associated with survival in transformed lymphoma (TL) and the prognosis has been generally poor. The R-IPI has been shown to be prognostic in the pre rituximab era.
To assess R-IPI as prognostic at lymphoma transformation in the rituximab era.
Patients with a diagnosis of diffuse large B-cell lymphoma transformed from LG-NHL (DLBCL-TL) were identified between January 2001 and December 2011 through the Moffitt Cancer Center Total Cancer Care Database. LG-NHL included follicular lymphoma (FL), marginal zone lymphoma (MZL), mucosa associated tissue lymphoma (MALT) and other low grade histologies. Patients with small lymphocytic lymphoma (SLL) with Richter’s transformation were excluded. All patients received rituximab based chemotherapy at transformation. Clinical data, pathologic data include morphology and immunohistochemistry (IHC) including CD10, BCL6, MUM1/IRF4 were recorded. Overall survival (OS) was calculated from the date of transformation. OS was estimated by the Kaplan-Meier method and compared using the long-rank test. A p-value< 0.05 was considered statistically significant.
A total of 81 patients were identified with DLBCL-TL. At diagnosis and transformation the median ages were 60 and 64 years (22 – 89), respectively. The male:female ratio was 0.72. The most common LG-NHL diagnosis was FL (75.3%). The median time to DLBCL transformation (TTT) was 3.4 years. At LG-NHL diagnosis 67.9% of patients were stage III/IV, 23.5% had bulky disease, 35.8% had extranodal disease (ED) and 14.8% were FLIPI1 score > 3. At transformation 29.6% had B symptoms, 77.8% had stage III/IV disease, 25.9% had ED, and 40.4% had an elevated LDH. DLBCL-GCB as per Hans algorithm was present in 65.5% of cases at transformation. The mean hemoglobin (Hb) and serum albumin (SA) level at transformation were 12.6 g/dl and 3.9 g/dl, respectively and an IPI > 3 was present in 22.2% of cases. R-IPI categories were very good in 4.9%, good in 72.8% and poor in 22.2%. Patients received rituximab prior to transformation in 65.4% with R-CHOP being the most common regimen used (84%). Radioimmunotherapy (RIT) was given in 17.3% of patients. Patients received 3 or more treatment lines in 74.1%. Patients underwent autologous and allogeneic stem cell transplant in 24.7 and 2.5% of cases, respectively.
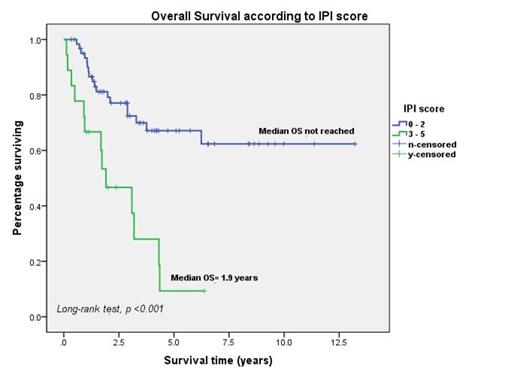
The median OS was 6.2 years. Poorer OS was associated with R-IPI > 3 at transformation (median OS 1.9 y, HR 2.9 [CI 1.5 – 5.9], p<0.0001) (Figure 1), FLIPI1 score 3 or more (median OS 1.7y, HR 2.9 [CI 1.7 – 5.1], p<0.0001), TTT< 2 years (median OS 2.8y, HR 3.2 [0.9 – 10.5], p=0.041), B symptoms (median OS 2.8y, HR 3.1 [1.5 – 6.4] p=0.003) and elevated LDH (median OS 2.8y, HR 2.6[1 – 6.6], p=0.04). The median OS with IPI< 2 was not reached. No survival differences were seen with FL vs non FL histology, older age, extranodal disease, bulky disease, use of RIT, number of treatment lines or rituximab prior to TL. There was a trend towards poorer OS with SA< 3.7 g/dl (median OS 2.8y, p=0.068).
An R-IPI >3 at transformation was associated with poorer OS in patients with LG-HNL who undergo histological transformation into DLBCL and treated with chemoimmunotherapy. This suggests that R-IPI can be used at the time of transformation to better assess the aggressiveness of disease. A confirmation of these findings will be needed in multicenter and prospective cohorts.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal