Abstract
Serum beta-2 microglobulin (β2MG) is an HLA class I protein. Its concentration is determined mainly from lymphoid tissue. Previous reports demonstrated that serum β2MG levels tend to increase with the stage of Hodgkin lymphoma (HL; Eur. J. Cancer. 1979; 15: 791-796: Cancer. 1980; 45: 318-326). Thus, this retrospective study aimed to examine the prognostic value of serum β2MG levels in HL.
We analyzed the data of 67 patients with previously untreated HL whose serum β2MG levels had been evaluated at diagnosis and who were treated at 7 institutions of the Yokohama City University Hematology Group between 1998 and 2011. We assessed the associations between survival and serum β2MG levels, all factors comprising the international prognostic index (sex, age, Ann Arbor stage, albumin levels, hemoglobin levels, white blood cell counts and lymphocyte counts at diagnosis), performance status, lactate dehydrogenase levels, and number of extra-nodular lesions, using univariate and multivariate analyses.
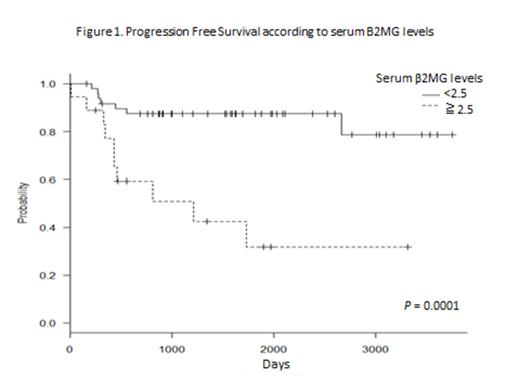
The patients included 40 men and 27 women with a median age of 41 years (range, 16- 81 years). The HL subtype was nodular sclerosis classical HL in 37 patients, mixed cellular classical HL in 23 patients, lymphocyte-rich classical HL in 6 patients, and nodular lymphocyte-predominant HL in 1 patient. The Ann Arbor stage of HL was stage I in 9 patients, stage II in 30 patients, stage III in 19 patients, and stage IV in 9 patients. All the patients were treated with doxorubicin, bleomycin, vinbrastine, and dacarbazine (ABVD) therapy alone (n = 37) or ABVD therapy plus involved-field radiation therapy (IFRT; n = 30). The clinical stage of HL in the patients treated with ABVD therapy alone was stage II in 11 patients, stage III in 17, and stage IV in 9. The clinical stage of HL in the patients who received ABVD plus IFRT was stage I in 9 patients, stage II in 19, and stage III in 2. The median observation period in the surviving patients was 53 months (range, 5- 123 months). The 4-year progression-free survival (PFS) and overall survival (OS) rates of all 67 patients were 76% and 89%, respectively. Thirteen patients had disease progression after treatment of HL. In total, 9 patients died: 3 of recurrent lymphoma, 2 of infection, 1 of acute circulatory failure during chemotherapy for HL, 1 of secondary malignancy, 1 of brain hemorrhage, and 1 of pulmonary chronic graft versus host disease. The patients with serum β2MG levels ³2.5 µg/mL showed inferior PFS (n = 18; 4-year PFS rate, 42%) compared to those with serum β2MG levels below<2.5 µg/mL (n = 49; 4-year PFS rate; P = 0.0001; Fig.1). In addition, the same trend was observed in the 4-year OS at a rate of 60% versus 98%, respectively (P = 0.001). When the patients treated with ABVD therapy alone and those treated with ABVD plus IFRT were respectively assessed, serum β2MG levels ³2.5 µg/mL were associated with inferior PFS in both groups of patients (P = 0.007 and P = 0.02, respectively). In the multivariate analysis, only serum β2MG levels ³2.5 µg/mL were correlated with poor PFS (P = 0.02) and poor OS (P = 0.03).
Therefore serum β2MG level at diagnosis is a useful prognostic marker for patients with HL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal