Abstract
The assessment of platelet function is crucial during the course of essential thrombocythemia (ET), as this myeloproliferative disorder is associated with concomitant thrombotic and bleeding complications. In the context of high platelet count, the assessment of platelet function is challenging. Current recommendations suggest the adjustment of platelet count for functional assays. This adjustment does not take into account the entire pool of circulating platelets in patients. This may explain the lack of predictive value of such assessment towards bleeding/thrombotic risk. Our objective was: 1- to set up a new strategy to evaluate platelet function, taking into account the circulating pool of platelets; 2- to evaluate the effect of JAK-2 mutation and of cytostatic treatment on platelet function.
Fifty two patients presenting with essential thrombocythemia (ET) were enrolled. ET diagnosis was established according to WHO criteria. Seventeen males and 35 females were included (sex ratio = 0.48, mean age 52 ± 16 years old). Fifteen healthy subjects were enrolled according to the hospital policy. Platelets were analyzed in whole blood flow cytometry (Beckmann-Coulter). GPIIbIIIa, GPIb and P-selectin were quantified on resting and TRAP-activated platelets (Platelet GP Receptors, Diagnostica Stago). Calculation for quantification strictly followed the manufacturer’s instructions and results were expressed as a number of GPs/P-selectin per platelet (mode A). In order to take into account the total amount of platelets, we calculated the total number of GPs/ P-selectin x platelet count (mode B).
As vWF binding to GPIb is critical in the prevention of bleeding, we measured the capacity of platelets to bind vWF in response to ristocetin using an original and sensitive assay in flow cytometry. JAK2 V617F mutation analysis, cytostatic treatment and clinical events (bleeding and thrombosis) were recorded.
Data were expressed as median [interquartiles] and Mann-Whitney was used for statistical comparisons. p<0.05 was considered as statistically significant.
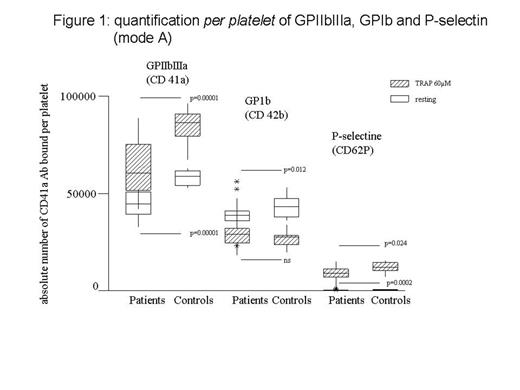
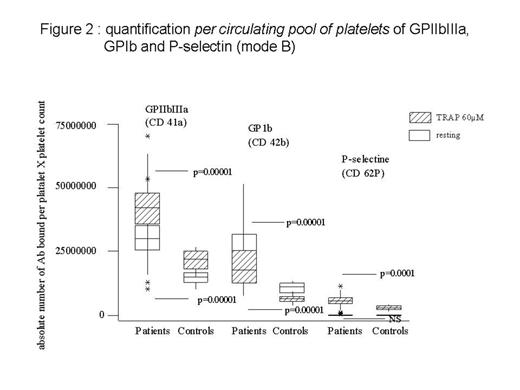
1) Comparison of two modes of quantification of GPs/P-selectin :
mode A (per platelet quantification): GPs and P-selectin expressed per platelet were reduced in patients versus controls (figure 1) (p<0.05),
mode B (per circulating pool of platelets) : total amount of GPs and P-selectin was much higher in patients (figure 2) (p<0.05).
2) vWF binding assay
Results showed a statistically significant defect of ristocetin-induced vWF binding to platelets in ET patients versus controls (p<0.05).
3) Effect of JAK-2 mutation
JAK-2 mutation was present in 23 patients. In this subgroup, platelet count was 748 G/L [555-912] (versus 560 G/L [500-750] in JAK-2 negative group, n = 27). In JAK2 + patients, the defect of GPIIbIIIa and of P-selectin per platelet (mode A) was more pronounced in comparison with patients without any JAK-2 mutation (p<0.05). On the contrary, when results were adjusted to the circulating platelet pool (mode B), total amount of GPs and P-selectin were not different according to the JAK-2 status. The expression of GPIb and the vWF binding were not affected by the JAK-2 mutation status.
4) Effect of cytostatic treatments :
We compared platelet function in patients under treatment (n=8, 480 G/L [402-912]) versus patients who were not treated by any cytostatic drug (n = 48, 693 G/L [531-903]). Interestingly, ristocetin-induced vWF binding was improved in treated patients (p<0.05). As a consequence, vWF binding recovered normal range.
5) Clinical events: Three patients experienced bleeding whereas 8 patients developed thrombosis (one had both events). Platelet function profile was not statistically different un these subgroups.
Our results show a platelet defect of GPIb, GPIIb-IIIa, P-selectin and vWF binding. On the contrary, when quantification of platelet receptors was adjusted to the pool of circulating platelets, values suggested a prohemostatic phenotype. The JAK-2 status influences the defect severity per platelet of GPIIb-IIIa and P-selectin. Interestingly, we observed a defect in vWF binding in ET patients, which was normalized by treatment. Flow cytometry is adapted to assess platelet defect in ET. However, our results raise the question of the most relevant method of calculation (per platelet and per platelet pool) to predict clinical events.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal