Abstract
Systemic mastocytosis with associated clonal hematological non mast cell lineage disease (SM-AHNMD), though uncommon, is considered a distinct subcategory of systemic mastocytosis according to the 2008 World Health Organization classification. Prior studies indicate that acute myeloid leukemia with t(8;21) has a strong link to SM-AHNMD. Systematic investigation of systemic mastocytosis associated with chronic myelomonocytic leukemia (SM-CMML) is limited. Bone marrow clonal mast cell proliferation, without overt clinical presentation following CMML often poses a diagnostic challenge and treatment dilemma. The overall survival for SM or SM-AHNMD varies according to subcategories of AHNMD and/or the therapeutic strategies taken. With hypomethylating agents becoming standard therapy for CMML with median overall survival (OS) of 12 to 24 months, acquisition of clonal mast cell proliferation may result in earlier relapse or refractoriness to conventional therapy. We reviewed the clinicopathologic features, cytogenetic and molecular findings, and clinical course of 10 patients with SM-AHNMD specifically chronic myelomonocytic leukemia (SM-CMML).
This retrospective study followed the guidelines of the Institutional Review Board (IRB). Cases diagnosed as SM-AHNMD at Moffitt Cancer Center from 1996 to 2013 were retrieved from the hospital electronic medical record and Cancer Registry. The diagnosis of SM- CMML was confirmed by histomorphology, laboratory data, phenotypic and molecular findings using current WHO criteria. Cases selected were CMML with concurrent or subsequent identification of a clonal mast cell proliferation (SM-CMML). Both solitary SM and SM-AHNMD other than CMML were excluded from this study.
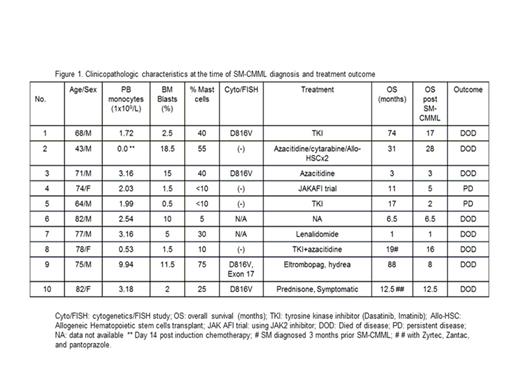
Forty patients diagnosed with indolent, cutaneous or systemic mastocytosis were identified, of which 19 were SM- AHNMD. Among the 19 patients, 10 qualified for the study, based on the above criteria, with a median age of 71.4 years (range 43-82) and male: female ratio of 7:3. Nine of 10 patients had no prior evidence of extramedullary mast cell involvement. In one patient systemic lesions were identified 3 months prior to the diagnosis of CMML. Two patients were originally diagnosed with myelodysplastic syndrome [Refractory cytopenia with multilineage dysplasia and Refractory anemia with excess blasts-2], which subsequently were diagnosed as CMML-1 and CMML-2, respectively. The length of time from the original CMML presentation to the diagnosis of SM-AHNMD was widely variable ranging from concurrent to over 80 months. All cases fit the WHO major criterion of aggregates of spindled mast cells. In addition all cases stained positive for CD117 and mast cell tryptase and displayed aberrant staining with either CD2 and/or CD25. Serum tryptase was also elevated (>20ng/ml). Standard treatment protocols with azacitidine were used for CMML. After the diagnosis of SM-AHNMD was rendered the treatment strategies were variable. Key clinical and pathologic features at the time of diagnosis of SM-CMML along with treatment and outcome are summarized in Figure 1. Laboratory values at the time of CMML diagnosis are not shown. The median overall survival was 14.75 months (range 1.0 to 88 months) after CMML was diagnosed and 7.25 months (range 1.0 to 28 months) following diagnosis of SM-CMML.
SM- CMML is a rare entity. Clinical presentation is extremely variable. The subtle morphologic features of a developing SM warrants careful histopathologic evaluation, judicious use of immunohistochemical stains and ancilliary techniques. Adherence to the current WHO criteria is important in the identification of these cases. Currently, established treatment guidelines for SM-AHNMD are non-existent. A large scale study is warranted to enrich physician experience in treatment of this rare entity and reduce the associated adverse outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal