Abstract
There is a growing tendency for drugs to be grouped according to their perceived ‘class effects’, regardless of the different pharmacological profiles of the parent drugs and of their metabolites. Imatinib, dasatinib, nilotinib, bosutinib and, most recently ponatinib, are approved tyrosine kinase inhibitor (TKI) therapies for chronic myeloid leukemia (CML), which are clinically efficacious as a result of ABL1/ BCR-ABL inhibition. Following their oral administration at standard therapeutic doses, the parent drugs are the major circulating species by area under the curve (AUC). However in the case of imatinib, dasatinib, bosutinib and ponatinib, the exposure of patients to major metabolites can be substantial compared to that of parent drug, with CGP74588 (which is much less active than imatinib against both BCR-ABL and KIT; Bioorg Med Chem 2013;21:3231) representing 10% of imatinib by AUC (Clin Pharmacokinet 2005;44:879); M20 and M24 representing 45 and 25% of dasatinib (Drug Met Disp 2008;36:1341), M2 and M5 representing 19 and 25% of bosutinib (Clinical Pharmacology Biopharmaceutics Review, http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm) and AP24600 representing 58% of ponatinib (Clinical Pharmacology Biopharmaceutics Review, http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm). Such major metabolites might make significant contributions to the on- and off-target effects of the parent drugs in vivoand may be responsible for some of the side-effects observed in patients. Here we report on the metabolism of the potent and selective BCR-ABL inhibitor, nilotinib and the preclinical profile of its major metabolites.
The metabolism of nilotinib was characterised in healthy subjects after oral administration of two capsules containing 200 mg [14C]-labelled nilotinib (50 μCi), and blood plasma, feces and urine samples were assayed in an appropriate scintillant either by counting an aliquot directly or after homogenisation, air-drying and solubilisation. Metabolites were characterised and quantified by HPLC with radioactivity detection and identified by mass spectrometry (LC-MS/MS) and, when possible, co-elution with non-radiolabeled authentic samples. Synthesised samples of the metabolites were evaluated in a large panel of assays for potential effects on kinase and non-kinase enzymes, G-protein coupled receptors, cell transporters, ion channels and nuclear receptors.
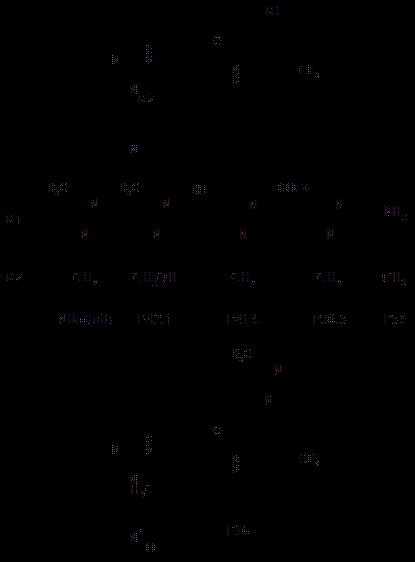
The oral absorption of nilotinib was determined to be ≥30% and excretion was mainly into the feces (93.5% of administered radioactivity), with neither nilotinib nor the identified metabolites being detected in the urine. Unchanged nilotinib was the major circulating component in human plasma, accounting for 87.5±9.2% of the total drug-related AUC. The main circulating metabolites were P41.6 (4.7% AUC), P36.5 (6.1% AUC), formed from oxidation of the methyl group in the methyl-imidazole moiety to a hydroxyl or carboxylic acid group, and P42.1 (1.3% AUC) resulting from oxidation of the phenyl-methyl group. Other, more minor metabolites included the pyridine N-oxide P36 and P50, resulting from degradation of the imidazole. All of the metabolites identified in humans were also observed in one or more of the animal species, employed for preclinical safety studies, with the exception of the minor fecal metabolites P38 (pyridine- + pyrimidine-N-oxide) and P40 (pyridine-N-oxide). In comparison to the parent nilotinib, which inhibits the BCR-ABL and KIT tyrosine kinases with mean cellular IC50 values of 20 and 217 nM, only P41.6 (19 and 284 nM), P42.1 (256 and 714 nM) and P50 (39 and 67 nM) exhibited kinase inhibition at concentrations < 2200 nM. In addition, none of the metabolites showed substantial activity at concentrations < 3000 nM against non-kinase targets.
Following oral administration of nilotinib to humans the predominant circulating species was the parent drug, with >15 minor and trace metabolites being identified. Given their in vitro potencies and target profiles, none of the metabolites are expected to contribute to the in vivo pharmacology of the parent nilotinib. This data further distinguishes the profile of nilotinib from other TKIs used for the treatment of CML.
Manley:Novartis Pharmaceuticals: Employment. Sheng:Novartis Pharmaceuticals: Employment. Tran:Novartis Pharmaceuticals: Employment. Kagan:Novartis Pharmaceuticals: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal