Abstract

Rapid eradication of blasts from peripheral blood during induction therapy in AML is associated with remission and overall survival. We prospectively evaluated the value of a bone marrow (BM) examination on day 5 of induction therapy in unselected newly diagnosed AML patients assigned for intensive induction. Seventy nine patients were enrolled during a 29-months period in six medical centers in Israel. BM blasts were evaluated by two independent observers and in most cases with the support of FACS analysis. Induction protocols administrated were 3+7 with daunorubicin 60 or 90 mg/m2 or clofarabine 40mg/m2 for five days [58 (73%), 10(13%) and 11(14%) patients, respectively]. Patients’ median age was 59 (range 22-78) years. Among surviving patients the actual follow-up time was longer than 9 months in 25(48%) patients and longer than 12 months in 16 (30%) patients. Cytogenetic results are available for 70 patients [2(3%), 47(67) and 21(30%) with standard, intermediate and poor risk, respectively]. Flt3ITD mutation was present in 11(13.9%) patients and NPM1 mutation, in 12 who presented with normal karyotype and were negative for FLT3-ITD.
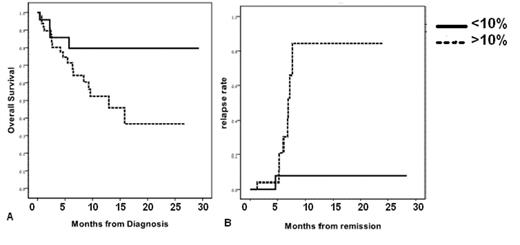
Treatment protocol was not altered on the basis of day 5 BM examination which was repeated on day 12-14. Residual disease (>10% blasts) was detected and a re-induction protocol (repeat 3+7 at doses of 60 or 45mg/m2 at day 14 or clofarabine 30mg/m2 on day 21) was administered in 20(25%) patients. Overall, 50(72%) patients achieved remission (CR1). Post-remission therapies varied according to patient age and risk factors. Overall, 29(37%) patients underwent allogeneic stem cell transplantation. During the study period, 27(34.2%) patients succumbed, 5(6.3%) during induction, 8(10%) while in remission and 12(15%) following relapse.
Bone marrow day 5 aspiration was not always informative and in seven cases where biopsy was not available the blast content couldn’t be assessed. Of the 72 patients with a valid day 5 blasts count, 24 (33%) were rapid responders in whom blasts were less than 10% of BM nucleated cells. On day 14, a lower than 10%, blast count was recognized in 54% of patients. However, 11/16 (69%) of patients who despite high blast counts at day 5 had a low count at day 14, either failed to achieve remission or relapsed. Only 5 patients presented with a low blast count at day 5 had a day 14 blasts count higher than 10%. Rapid response on day 5 was not associated with age or molecular status; yet, there was a trend (p=0.08) towards lower frequency of poor cytogenetics among these patients. Surprisingly, mean presenting WBC was higher among rapid responders.
Bone marrow blast count on the fifth day of induction during chemotherapy is a powerful predictor of AML prognosis, irrespective of other pre-treatment risk factors. Larger studies, with longer follow up are required to determine its role in clinical management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal