Abstract
Transfusions of packed red blood cell (pRBC) units to infants in Neonatal Intensive Care Units (NICUs) may predispose neonates to healthcare-associated infections (HAIs). We compared neonatal pRBC transfusion practices at four NICUs (Morgan Stanley Children’s Hospital of NewYork-Presbyterian, Columbia University Medical Center, Komansky Children’s Hospital of Weill Cornell Medical Center, Christiana Care Health System, and Children’s Hospital of Philadelphia). In addition, because prolonged refrigerator storage of pRBC may further predispose to HAIs, we tested the hypothesis that an increased mean RBC storage age was associated with a greater risk of infections.
The interdisciplinary NICU Antimicrobial Prescribing (iNAP) study was conducted in four Level III NICUs from May 2009 to April 2012 to assess HAIs and improve antimicrobial prescribing in NICUs. Eligible infants were admitted <7 days of age and hospitalized ≥4 days. Demographic (e.g., sex, birth weight [BW]) and clinical data (e.g., HAIs and surgical procedures) were collected. HAI included culture negative sepsis defined by treating clinicians, necrotizing enterocolitis, or bacteremia treated for ≥ 4 days. pRBC transfusions were collected from blood bank records at each site. Descriptive statistics were performed using GraphPad Prism 6.
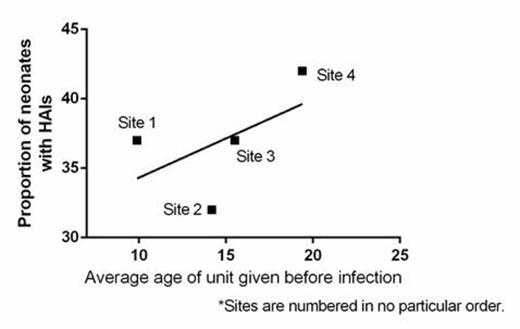
All sites used irradiated, leukoreduced, CMV negative pRBCs and practiced donor limitation. Blood bank preparation procedures were similar at all sites except that one site stored 3% of units in CPDA-1 in addition to units stored in Additive Solutions (AS), and another site irradiated the parent unit instead of the aliquot; the other sites irradiated the aliquot prior to release. During the study period, 6411 pRBC transfusions were administered to 1381 (21.5%) of 6184 enrolled infants. The transfusion rate was 12.6%, 37.3%, 16.7%, and 25.1% at sites 1-4, respectively. The rate of transfusion by normal BW (≥2500g), low BW (1500-2499g), very LBW (<1500g), and extremely LBW (<1000g) was 0.8, 0.4, 2.8, and 5.5 per patient, respectively. Transfused infants received an average of 4.7 transfusions (range 1-63; average of 3.5, 4.5, 4.5, and 6.0 transfusions at each respective site) with a mean donor exposure of 2.1 (range 1-23). Overall, 50% of pRBC transfusions occurred in the first 17 days of life and 34% occurred during the first week of life. Surgical and post-surgical transfusions accounted for 1389 (21.7%) of 6411 transfusions in 486 (35%) of 1381 transfused infants. Infants undergoing congenital diaphragmatic hernia repair required the most transfusions; 34 infants received 537 ECMO-related transfusions. The average storage age of the pRBC transfused was 16.1 days, but differed by site (12.5, 14.6, 16.7, 19.9 days for each site, respectively, p< 0.001 by Kruskal-Wallis test with Dunns Multiple Comparison Test) and by aliquot (1st-5th aliquot average age 12, 16, 19, 21, and 23 days, respectively). The average age of units transfused in infants without HAIs (n=5693) was 15.2 days; while the average age of units transfused in infants with HAIs (n=491) that developed after transfusion was 15.4 (p=0.04). An ecological study comparing all sites did not find a significant association between the average storage age of units transfused per site (excluding units transfused after onset of infection) and the proportion of neonates with HAIs at the site (R2=0.29; p=0.46; see Figure).
To our knowledge, this is the largest cohort study of neonatal transfusion practices in Level III NICUs. Transfusion practices were similar at each site. The average storage age of transfused pRBC units varied among the four sites; however, the mean RBC storage age of RBCs transfused to patients with or without HAIs was not markedly different and hospitals with a longer mean storage age did not have a higher proportion of neonates with HAIs. Further analysis is needed to explore the relationship between pRBC storage and HAIs, while controlling for differences in patient characteristics.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal