Abstract
Immune thrombocytopenia (ITP) is characterized by impaired megakaryocte production and maturation, as well as premature platelet destruction. The effect of this disease on platelet production is not clear. The Immature Platelet Fraction (IPF) is a novel parameter available on the Sysmex XE-Series Hematology analyzers. It can be expressed as both IPF percent (IPF %) and absolute IPF count (AIPF#). It has been shown that IPF% is higher in Immune Thrombocytopenia (ITP) than in the normal population, and is an indicator of bone marrow platelet production or thrombopoiesis.
To characterizes the IPF parameters in pediatric patients with ITP at diagnosis and during different phases of the disease (newly diagnosed, persistent, and chronic).
This is a retrospective, single institution study performed at a tertiary care pediatric hospital. We reviewed the medical charts and electronic databases of all patients with ITP who had measured IPF parameters between June 2011 and June 2013. The standard definitions and terminology of the International Working Group were used.
Patient age, phase of ITP at the time of the blood test (newly diagnosed, persistent, and chronic), initial platelet count, IPF%, AIPF#, and type of therapy given (including observation alone) were recorded. We then compared the platelet count, IPF%, and AIPF# between the ITP phases at the time of initial CBC and looked at the relationship between the platelet count and IPF%.
Comparisons between groups were performed using Kruskal-Wallis tests or Mann-Whitney tests, as appropriate. Association between measured blood parameters was measured using the Spearman correlation coefficient.
We included 47 patients; mean age was 9.4 years (1-18). At the time of the study,16 (34%) patients had newly diagnosed ITP (0-3 Months), 6 (12.8%) had persistent ITP (3-12 Months), and 25 (53.2%) had chronic ITP (>12 Months)
The initial platelet count was lower in newly diagnosed patients at 6x109/L (IQR 2-8), compared to patients with persistent ITP (16x109/L, IQR 7-24.5) and chronic ITP (30x109/L, IQR 17.5-53.5) (p=0.000).
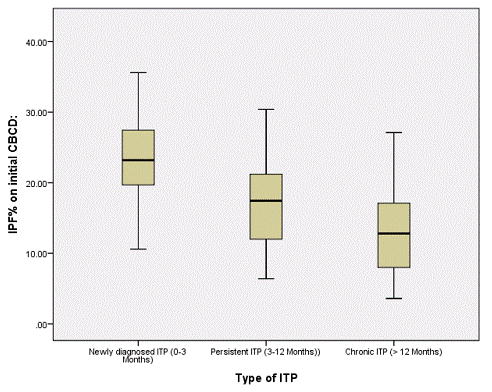
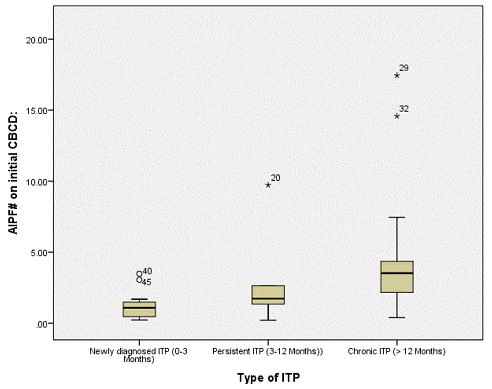
IPF% was significantly higher in newly diagnosed ITP at 23.2% (IQR 19.6-27.8) compared to persistent ITP (17.4%, IQR 10.6-23.5) and chronic ITP (12.8%, IQR 7.3-17.1, p=.001) (figure 1A). In contrast, AIPF# was significantly lower in newly diagnosed ITP (1.1x109/L, IQR 0.44-1.5) compared to persistent ITP (1.7x109/L, IQR 1.1-4.4) and chronic ITP (3.5x109/L, IQR 2.0-4.5, p<0.001) (figure 1B).
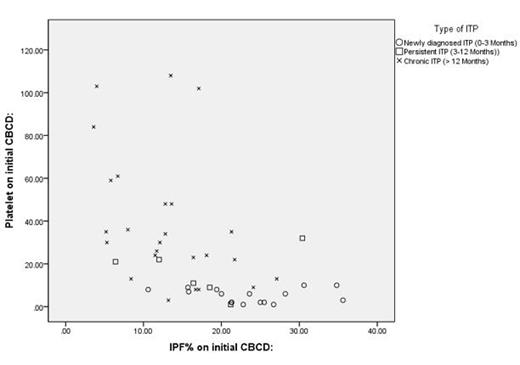
IPF% correlated negatively with platelet counts for all patients (P=0.001) and this correlation was significantly more prominent in chronic ITP (figure 2).
IPF parameters may be useful in understanding the mechanism of ITP through the evolution of the disease. From the time of diagnosis of ITP through progression to chronic ITP, there is a steady decrease in IPF% and increase in AIPF# .The high IPF% in the newly diagnosed setting suggests that megakaryocytes are still active, whereas the lower IPF% in chronic ITP indicates inhibition of megakaryopoiesis or a different underlying pathophysiology. This may have important clinical implications when considering TPO receptor agonist therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal