Abstract
Although thrombopoietin-receptor agonists have recently been introduced for the treatment of refractory immune thrombocytopenia (ITP), splenectomy is still the standard treatment option for patients with steroid-refractory ITP. However, open and laparoscopic splenectomy is associated with a mortality rate of 1.0% and 0.2%, respectively, and the major known long-term risk of splenectomy is severe bacterial sepsis. Partial splenic embolization (PSE) is an alternative to splenectomy for patients with steroid-refractory (Kimura et al., AJR 2002). PSE does not require general anesthesia and has not been associated with severe complications. In this study, we analyzed the efficacy and long-term outcomes of PSE in steroid-refractory ITP patients.
Between 1988 and 2009, 77 patients with chronic ITP [30 men and 47 women, 16.5–80.9 years old (median age, 46.5 years)] underwent PSE at Chiba University Hospital. Almost all patients did not respond to steroid treatment or other therapies including Helicobacter pylori eradication and immunosuppressive drugs. A 5-French catheter was introduced via the femoral artery to the middle splenic artery and a 0.089-cm guidewire was inserted coaxially. Embolization of intrasplenic arterial branches was performed by the injection of 2 x 2 mm fragments of Gelfoam and an antibiotic solution. Splenic embolization was monitored angiographically during the procedure, and embolization was stopped after 70% of the splenic parenchyma had been ablated. The therapeutic response to PSE was evaluated on the basis of the platelet (PLT) count at 1 year after PSE: a complete response (CR) was defined as PLT count of more than 10 x 1010/L without any medication and a partial response (PR) was defined as PLT count = 5–10 x 1010/L without any medication. Patients who required medication to maintain a PLT count of more than 5 x 1010/L or patients with a PLT count of less than 5 x1010/L were considered to have no response (NR).
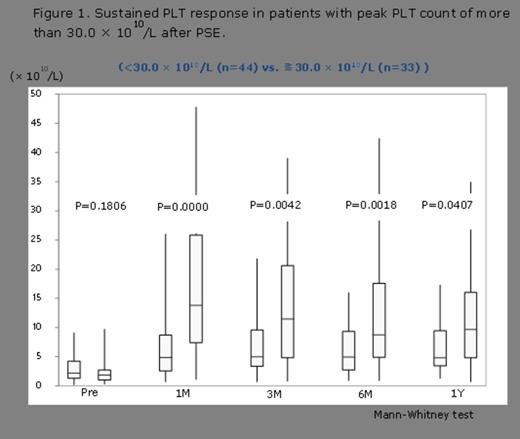
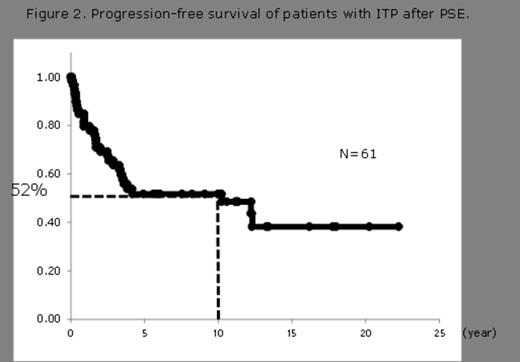
The average PLT count prior to PSE was 2.7 ± 2.4 x 1010/L. The mean time to achieve the peak PLT count was 10.2 ± 5.2 days after PSE. The PLT count was 11.1 ±10.3 x 1010/L (n = 74), 9.8 ± 8.3 x 1010/L (n = 70), 9.1 ± 8.2 x 1010/L (n = 65), and 9.1 ± 7.5 x 1010/L (n = 69) at 1 month, 3 months, 6 months, and 1 year, respectively. One year post PSE, CR or PR was obtained in 33 (58%) of the evaluable 57 patients and 24 patients (42%) had NR. The group in which the peak PLT count after PSE was over 30.0 x 1010/L showed a significantly higher PLT count than the group in which the peak count was under 30.0 x 1010/L after PSE treatment (Figure 1). The peak PLT count was significantly higher in CR and PR groups (37.4 x 1010/L) than in the NR group (15.0 x 1010/L) (p = 0.041). In addition, 52% patients did not require additional treatment for 10 years after PSE (Figure 2); in 16 patients, PSE was performed for the second time after recurrence; and CR or PR was obtained in 5 patients (31%). There were no severe PSE-related complications such as splenic abscess and no PSE-related deaths.
PSE might be a safe and effective alternative therapy to splenectomy for patients with steroid-refractory ITP as it generates long-term durable responses.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal