Abstract
Recent results from our prospective multi-center study identified patients with t (8; 21) AML as high-risk according to their MRD status after the second consolidation chemotherapy and allo-HSCT can benefit this part of patients; however, the relapse rate was reported to be 22% even after allo-HSCT for those high-risk patients. To date, there have been no studies to answer the question of whether the specific fusion gene, RUNX1/RUNX1T1 can be used to further distinguish between patients with low and high risks of relapse in allo-HSCT setting, just like the already established standard for MRD measurement in CML and APL.
Sixty consecutive AML patients with t (8; 21) and identified as high-risk according to the criteria from our recently published report patients who received allo-HSCT were enrolled between January 2006 and January 2013. Serial MRD monitoring by RQ-PCR post HSCT was done. The impact of MRD monitoring on transplant outcomes was assessed.
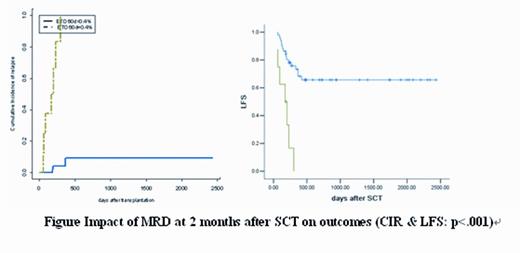
A > 3 log reduction at 1 month after HSCT in RUNX1/RUNX1T1 transcripts from diagnosis, is associated with 2-year CIR of 17% in the 88% of patients achieving it, compared with 43% in the remaining (p=.02). A > 3 log reduction at 2 months after HSCT in transcripts from diagnosis, is associated with a CIR of 9% and LFS of 66% in the 86% of patients achieving it, compared with CIR of 100% and LFS of 0% in the remaining (both p<.001). A > 3 log reduction at 3 months after HSCT in RUNX1/RUNX1T1 transcripts from diagnosis, is associated with a CIR of 11% and LFS of 73% in the 78% of patients achieving it, compared with CIR of 44% and LFS of 0% in the remaining (both p<.001). Of the 60 patients analyzed, 28 patients had positive MRD, occurring at a median of 110 days (30-540 days) after transplant. The predictive value of sequential monitoring could be demonstrated in 8 patients culminating in clinical relapse (representing 73% of all relapsing patients). The median time from MRD positivity in BM to morphological relapse was 95 days (range, 33-140 days).
A > 3 log reduction at the first 3 months after HSCT in RUNX1/RUNX1T1 transcripts from diagnosis is highly prognostic. We conclude that MRD monitoring by RQ-PCR at regular early time points post HSCT in t (8; 21) AML allows further identification of patients at high risk of relapse even after allo-HSCT and could now be incorporated in clinical trials to evaluate the role of risk directed prophylactic/preemptive therapy.
This work was partly supported by The Key Program of National Natural Science Foundation of China £¨Grant No. 81230013£©, Beijing Municipal Science & Technology Commission (No.Z121107002812033) and Bejing Municipal Science & Technology Commission£¨No.Z111107067311070).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal