Abstract
Bendamustine is a novel active agent in CLL with favorable safety profile. We have previously reported the outcomes of allogeneic stem cell transplantation (alloSCT) in CLL after FCR conditioning (Khouri et al. Cancer 2013). More recently, we initiated a trial with BFR. Herein, we compare outcomes in relapsed/refractory CLL patients following alloSCT according to the conditioning regimen received.
We studied 101 CLL patients treated on 3 consecutive trials at our center between 1999 and 2012. 75 (74%) received FCR and 26 (26%) received BFR. The BFR regimen consisted of bendamustine 130 mg/m2 IV daily on days -5 to - 3 prior to transplantation, thus substituting the cyclophosphamide in the FCR regimen. The dose and schedule of fludarabine (30 mg/m2 IV daily x3) and rituximab (375 mg/m2 IV on day –13 and 1000 mg/m2 on days -6, +1, and +8) were similar in both regimens. Tacrolimus and mini-methotrexate were used for GVHD prophylaxis. In addition, thymoglobulin 1 mg/kg IV was given on days -2, and -1 in patients receiving an unrelated donor transplant. Patients were staged with CT, PET (whenever indicated) scans and marrow biopsies, every 3 months for the first year, every 6 months x 5 years, then yearly thereafter. Minimal residual disease (MRD) by multicolor flow cytometry using an international standard approach was also assessed from bone marrow samples since 2004.
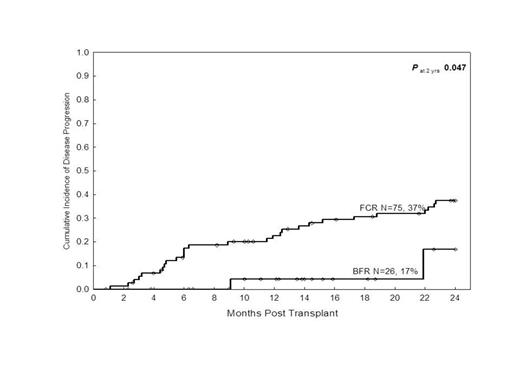
Patients characteristics were similar in both groups. This included median age (58 years in both), sex distribution, and median number of prior therapies (3 in both), β2-microglobulin >3 mg/L, refractory disease (38% in BFR vs. 46% in FCR, P=0.5), presence of 17p deletion [27% in BFR and 11/30 (37%) in FCR], and peripheral blood stem cell source (92% and 89%, respectively). More patients however received their transplants from unrelated donors in the BFR group than the FCR group (54% vs. 27%, respectively, P=0.01). Treatment-related mortality was similar within the 2 groups [4% and 7% at 6-months; 8% and 16% (P=0.3) at 1-year]. The incidence of acute grade 3 GVHD was 4% and 8% in the BFR and FCR groups, despite the higher % of unrelated transplants in BFR. None had acute grade 4 GVHD in either group. Median follow-up time for BFR and FCR groups were 14 (range 4-48), and 76 (range, 24-195) months, respectively. The 2-year progression rates in the BFR and FCR were 17% vs. 37%, respectively (P=0.04) (Figure), and the 2-year PFS rates were 75% vs. 40%, respectively (P=0.01). There was also a trend for a better 2-year OS rates (92% vs. 68%, P=0.1), favoring the BFR group. The conditioning regimen (P=0.04) and β2-microglobulin >3 mg/L (P=0.03) were the only predictors for progression by uni- and multivariate analysis undertaken in all 101 patients, whereas a number of prior therapies of > 3 was the only predictor for OS. Recent studies have suggested that MRD is an independent predictor of PFS and OS in CLL after conventional chemotherapy as well as after alloSCT. We assessed MRD in 61 patients following alloSCT. A 6-months landmark analysis showed that MRD-negativity was not a predictor for progression in these patients (P=0.6). Last MRD tests before clinical progression dates was available for 22 of 39 progressions in the FCR/BFR group. Last MRD test was found to be negative in 14/22 relapsed patients. Median duration between last MRD-negative test and clinical relapse was 92 days (range, 1-725). Median duration between last MRD-positive test and clinical relapse was 71 days (range, 21-330)
Our results show a lower rate of progression and improved survival after BFR when compared to FCR regimen in alloSCT for CLL. MRD by multicolor flow cytometry was not able to predict risk of progression in these patients whose disease was also assessed by CT imaging following transplantation.
Khouri:Cephalon: Research Funding. Off Label Use: Bendamustine in transplantation.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal