Abstract

Treatment of AL amyloidosis (AL) has typically followed the treatment patterns used in myeloma, but has changed in a disease specific manner during the past few years with increasing use of Melphalan-Dexamethasone (MD) combination as well as bortezomib (Btz) and IMiD based regimens. It is not clear how the more recent approaches have impacted the outcome of patients with AL.
We reviewed the medical records of 555 patients with AL seen at Mayo Clinic between Jan 2004 and Dec 2010 and within 30 days of diagnosis. Details regarding the laboratory findings, treatments and response to therapy were extracted by a review of their medical records and from an existing database. We further grouped patients into two groups: those diagnosed during the initial half (Jan 2004 to June 2007) and those diagnosed after that (July 2007 to Dec 2010) to study time trends in survival and treatment patterns.
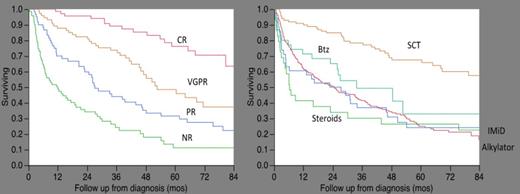
The median estimated follow up for the entire group was 67 months (95% CI; 59, 72) and 182 (33%) were alive at the time of analysis. The median age was 64 years (range; 32-95). The median overall survival (OS) for the entire cohort was 21 months and was nearly identical for the patients included in the two time groups; P=0.5. The 2-year mortality was 52% for both groups. The median OS was NR, NR, 24 mos. and 6 mos. respectively for patients in the revised Mayo stages 1, 2, 3, and 4. Treatment details/ follow up were either not available or no treatment was employed for 131 (24%) patients. The median OS for this group was 3 mos. compared with 36 mos. for the rest. The first line of therapy was alkylator based (mostly Mel-Dex) in 212 patients (51%), autologous transplant (SCT) in 99 (24%) patients, IMiD based in 37(9%), Btz based in 36 (9%) and steroid based in 29 (7%). Comparing the two time periods, the treatments were similar with the following exceptions: 32/36 patients receiving Btz based therapy were in the later group; and 26/29 patients treated with steroids alone were in the former group. A hematologic response could be determined in 275 (65%) patients; with the best response of CR (17%), VGPR (18%), PR (14%) and no response (17%). The median OS from diagnosis for these response categories were 99, 53, 27 and 12 mos respectively (p<0.01). A VGPR or CR was seen among 55%, 39%, 29%, 26% and 10% respectively in patients treated with SCT, Btz, Alkylators, IMiDs and steroids. The median OS from diagnosis was 99, 34, 25, 25, and 6 months respectively for patients treated with SCT, Btz, Alkylators, IMiDs and steroids, P<0.01 (Figure). The results were similar using a 4-month landmark to exclude patients who have not had adequate time to respond. Among the 146 patients evaluable for an NT-PRoBNP response, patients with a decrease of 30% had median OS that was not reached compared with 27 mos for those failing to achieve the response (4 month landmark).
The current data form a more recent cohort of patients seen at a single referral institution serves to highlight the shift in the therapeutic approaches, with the increased use of Btz based combinations. The results confirm the prior observations of the impact of hematologic response depth and outcome as well as the effect of an NT-ProBNP response. While patients undergoing SCT have a better outcome, likely a result of the selection bias of excluding high-risk patients from SCT, the OS do not appear significantly different between patients receiving alkylator therapy, IMiD based therapy or Btz based therapy. The lack of difference may also reflect the relatively shorter follow up s well as the small numbers of patients in each group.
Kumar:Celgene: Consultancy, Research Funding; Millennium: Consultancy, Research Funding; Onyx: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal