Abstract
Non-infectious transplant-related complications (TRC) early after allogeneic hematopoietic cell transplantation (allo-HCT) are associated with considerable morbidity and mortality. Recently, research interests have been focused on endothelial cell (EC) dysfunction and angiogenesis which is a common feature implicated in the pathogenesis of TRC. Angiopoiein-2 (ANG2) plays an essential role in promoting endothelial instability in the process of angiogenesis and predisposing tissue damage. Recent studies have indicated that high level of ANG2 is associated with graft-versus host disease (GVHD) but the role of ANG2 in TRC remains unclear. Thus, we evaluated the association between plasma ANG2 levels and TRC.
Patients who received allo-HCT between 2000 and 2012 and had available blood samples at transplant (day0) were included in the analysis. Patients who had undergone any prior transplantation within one year were excluded. A total of 153 patients were evaluated and the median age of patients was 49 years (range: 16-68). TRC was defined as sinusoidal obstruction syndrome (SOS), systemic transplant-associated microangiopathy (TAM), capillary leak syndrome (CLS) and grade III/IV acute GVHD with massive fluid retention or hemophagocytic syndrome (HPS). Plasma ANG2 levels were measured by ELISA kit and we set the cut-off value of 2.0ng/mL for ANG2 at transplant. Multiple characteristics including ANG2 were evaluated for their association with TRC, GVHD and overall survival (OS).
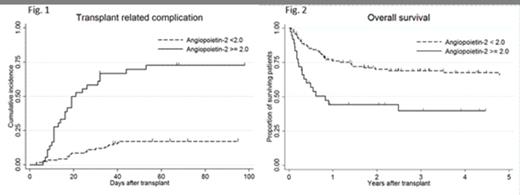
Median follow-up duration of surviving patients after transplant was 5 years. Seventy percent of the patients received allo-HCT for acute myeloid leukemia or myelodysplastic syndrome and the disease risk was high (not in remission) in 38% of the patients. Sixty-five percent of the patients received allo-HCT from unrelated donor and the source of graft was HLA-matched in 53%, mismatched in 18%, and cord blood in 29% of the patients. Seventy-five percent of the patients received myeloablative conditioning regimen and 67% of the patients received GVHD prophylaxis with tacrolimus. ANG2 level at the onset of TRC was significantly higher compared to the peak levels of the patients who had no complication during the transplant (control) {median of ANG2 ng/ml (range): control, 2.5 (1.4-4.0); TRC, 6.4 (2.4-15.7), p<0.001}. ANG2 was not elevated at the onset of pre-engraftment immune reaction, engraftment syndrome, HPS, and documented bacterial infection. Twenty-four percent of the patients showed ANG2 level of more than 2.0ng/mL at transplant and multivariate analysis with logistic regression revealed that male, more than 10% of blast in the bone marrow at the transplant and conditioning regimen with melphalan were significantly associated with high ANG2. Cumulative incidence of TRC at day100 after transplant was 30% and 48% of these patients also experienced grade III/IV acute GVHD during the transplant. Cumulative incidences of TRC at day100 after transplant for patients with or without high ANG2 were 73% and 17%, respectively (Fig. 1). Univariate analysis with Cox proportional hazard model revealed that high ANG2 at transplant was significantly associated with the risk of latter TRC (Hazard ratio [HR]: 6.9, p<0.001) but was not associated with the risk of grade III/IV acute GVHD (HR: 1.5, p=0.327). Multivariate analysis revealed that transplant from unrelated donor (HR: 3.1, p=0.052) and high ANG2 (HR: 11.8, p<0.001) were independently associated with the risk of TRC. One-year overall survivals after transplant for patients with or without high ANG2 at transplant were 42% and 74% (Fig. 2). High ANG2 was also an independent risk factor for OS (HR: 2.9, p=0.006) along with high disease risk at transplant (HR: 2.0, p=0.008) and transplant from unrelated donor (HR: 2.2, p=0.036).
High plasma ANG2 at transplant was significantly associated with TRC but not with grade III/IV acute GVHD. High ANG2 at transplant could serve as a potential risk marker for latter TRC and inferior survival. Further investigations are needed for prevention strategies for TRC navigated by plasma ANG2.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal