Abstract

Daily prednisone is considered standard first line therapy in idiopathic thrombocytopenic purpura (ITP). Since its long-term efficacy is limited, other glucocorticosteroids and schedules have also been tested. The most widely used regimen is pulsed dexamethasone. We performed a randomized, prospective, multicentre trial to analyze the efficacy of daily prednisone versus pulsed dexamethasone as first line treatment of ITP.
Diagnosis was made and requirement for treatment defined as outlined in the 1996 practice guidelines of the American Society of Hematology (Blood 88:3, 1996). The primary endpoint was remission duration, remission being defined as any platelet count above 50x109/l. Sample size calculation was based on the assumption that 60 % of patients receiving daily prednisone and 90 % of patients receiving pulsed dexamethasone would achieve a remission. To detect an increase in the percentage of responding patients maintaining remission for at least 6 months from 35 % to 70 % at a significance level of 5 % with a power of 80 %, 22 patients had to be included in each treatment arm. The trial was approved by the Ethics Committee of the Medical Faculty of the University of Duisburg-Essen, Germany (no. 02-1900; May 13, 2002) and registered with and approved by the Federal Institute for Drugs and Medical Devices, Bonn, Germany (BfArM no. 4019209; July 22, 2002).
During the first week of treatment all patients received prednisone (1 mg/kg/d) followed by a 1:1 randomization between daily prednisone and pulsed dexamethasone. In the prednisone arm prednisone was given at 1 mg/kg/d for another week. In case of remission the dose was gradually tapered over a course of 19 weeks to reach a maintenance dose not exceeding 25 mg/d at the end of week 13 and below 7.5 mg/d at the end of week 19. If remission was not achieved after a total of two weeks of daily prednisone at 1 mg/kg, the dose was increased to 2 mg/kg/d for another 2 weeks. In case of remission the dose was subsequently reduced as described above. Patients randomized to the dexamethasone arm were treated with 6 courses of pulsed dexamethasone (0.6 mg/kg day 1 to 4) at 3-week intervals. In case of failure to achieve a remission patients crossed over to the alternative treatment arm (prednisone: no remission after 4 weeks of prednisone at 1-2 mg/kg/d, maintenance dose above 25 mg/d at the end of week 13 or above 7.5 mg/d at the end of week 19; dexamethasone arm: no remission after two cycles).
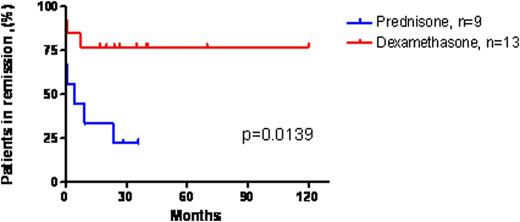
Recruitment was stopped before reaching the target patient number because of slow accrual and an inability to extend the study subject insurance. Between 2002 and 2010 26 patients were enrolled. Twelve patients were randomized to prednisone, 14 to dexamethasone and 4 were subsequently excluded because of protocol violations (3 in the prednisone and 1 in the dexamethasone arm). The median age in the 22 evaluable patients was 45 years (range 22 – 77), 13 were male, 18 had primary and 4 had secondary ITP. All patients achieved a remission. There was no statistically significant difference in the interval between treatment initiation and achievement of remission (p=0.55). Remission duration, however, was significantly longer in the dexamethasone as compared to the prednisone arm (p=0.0139; Figure 1). Median treatment duration in the prednisone arm was 85 days (range: 28 – 153), and median number of treatment cycles in the dexamethasone arm was 5 (range: 3 – 7). During the treatment the median cumulative cortisol equivalent dose was 15.780 mg in the prednisone and 34.560 mg in the dexamethasone arm. Grade 3 or 4 bleeding events during treatment were limited to petechiae (prednisone: 1 patient; dexamethasone: 2 patients). Grade 3 or 4 adverse events were recorded in 1 patient in the prednisone arm (hypertension) and 2 patients in the dexamethasone arm (hyperglycemia, hypokalemia).
Remission duration (platelets >50x109/l) in ITP patients receiving daily prednisone versus pulsed dexamethasone
Remission duration (platelets >50x109/l) in ITP patients receiving daily prednisone versus pulsed dexamethasone
In this randomized trial sequential cycles of pulsed dexamethasone proved more effective than continuous daily prednisone in inducing stable remission in treatment naïve patients with ITP. This correlated with a higher cumulative glucocorticosteroid dose. We hypothesize that the intensity of immunosuppression is an important determinant of treatment outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal