Abstract
Recent practice guideline changes suggest all patients with MM should receive bisphosphonates, regardless of the presence of bone disease. Nitrogen-containing bisphosphonates, ZA and PAM, inhibit protein prenylation, a process crucial for osteoclast survival. This inhibition also interferes with tumor cell adhesion, angiogenesis, and proliferation suggesting potential for anti-tumor activity of bisphosphonates. Morgan et al showed increased OS with use of ZA versus clodronate in MM. This increase was independent of the effect on bone disease, supporting anti-tumor activity of ZA. ZA and PAM are the two approved bisphosphonates for MM in the United States. In in-vitro studies, ZA has increased potency compared to PAM, a finding that may result in increased apoptosis of tumor cells. A meta-analysis by Mhaskar et al demonstrated an association between higher bisphosphonate potency and improved OS in MM. In an effort to clarify the effect of ZA versus PAM on OS in MM, we evaluated outcomes in a large cohort of United States Veterans with MM.
We identified 1,018 patients with newly diagnosed MM in the Veterans Administration Cancer Registry between 2002 and 2009, who were treated with either PAM or ZA, but not both. Data was collected on age, co-morbidities, date of diagnosis and death, myeloma specific and supportive medications, and baseline lab data. Cox proportional-hazards was used to assess association between bisphosphonate use and OS while controlling for other prognostic factors. Propensity score analyses were performed to reduce confounding by indication, using the inverse probability weighting (IPW) approach of Cole and Hernan and propensity score matching. The covariates for each propensity model were the same as those in the main analysis.
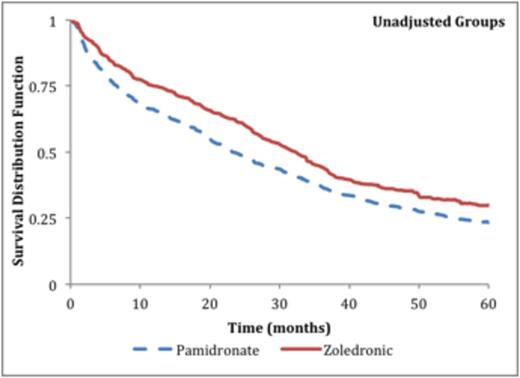
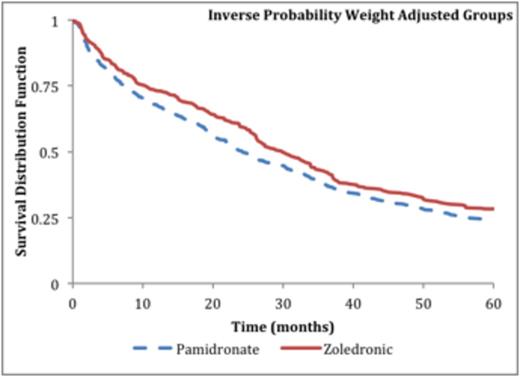
Of the 1,018 patients in the cohort, 383 received ZA and 635 received PAM. The median follow-up was 26.9 months. After adjustment using propensity score groups, baseline characteristics were well balanced between the groups (Table 1). Kaplan-Meier curves showing OS of patients receiving ZA versus PAM are shown in Figure 1. After controlling for age, weight, comorbidity score, era of diagnosis (before or after 2006), baseline lab characteristics, and treatment, OS was significantly improved with ZA compare to PAM (HR 0.84; 95% CI, 0.72-0.98). In both the IPW and propensity score matching analyses, ZA significantly improved OS in MM (HR 0.84; 95% CI, 0.72-0.97) and (HR 0.83; 95% CI, 0.69-0.99) respectively.
Baseline Characteristics
| . | Unadjusted Data . | Adjusted with IPW . | Propensity Score Matching . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| . | PAM . | ZA . | P-value . | PAM . | ZA . | P-value . | PAM . | ZA . | P-value . |
| Age (mean) | |||||||||
| Male Sex (%) | 98 | 96.1 | 0.0773 | 97.3 | 97.1 | 0.8304 | 96.6 | 96.6 | 1.0000 |
| Race (%) | |||||||||
| White and other | 74.5 | 70 | 72.8 | 73 | 70.5 | 71.6 | |||
| Black | 25.5 | 30 | 0.1169 | 27.2 | 27 | 0.9381 | 29.5 | 28.4 | 0.7397 |
| Mean Charlson score | 2.6 | 2.4 | 0.1851 | 2.6 | 2.5 | 0.3721 | 2.6 | 2.4 | 0.3503 |
| Transplant (%) | 15.6 | 11 | 0.0385 | 13.7 | 13.8 | 0.9591 | 11.4 | 11.4 | 1.0000 |
| Melphalan_use (%) | 35.3 | 36.8 | 0.6199 | 36.2 | 35.5 | 0.8112 | 38.4 | 36.7 | 0.6404 |
| Lenalidamide_use(%) | 21.7 | 27.4 | 0.0394 | 23.4 | 23.9 | 0.8532 | 24.7 | 27.6 | 0.3910 |
| Thalidomide_use(%) | 51.3 | 52.7 | 0.6643 | 51.5 | 51.3 | 0.9396 | 51.1 | 52.8 | 0.6508 |
| Steroid Alone (%) | 22.7 | 16.2 | 0.0125 | 20.5 | 20.8 | 0.9133 | 19.0 | 17.1 | 0.4926 |
| Bortezomib_use(%) | 34.3 | 32.9 | 0.6397 | 33.7 | 32.9 | 0.7836 | 34.1 | 33.2 | 0.8109 |
| Hemoglobin (mean) | 10.7 | 10.7 | 0.7442 | 10.8 | 10.6 | 0.1493 | 10.9 | 10.7 | 0.2788 |
| Creatinine (mean) | 1.9 | 1.8 | 0.0012 | 1.8 | 1.9 | 0.5361 | 1.5 | 1.6 | 0.7944 |
| Albumin (mean) | 3.3 | 3.3 | 0.8803 | 3.3 | 3.2 | 0.6517 | 3.3 | 3.2 | 0.6348 |
| Calcium (mean) | 9.7 | 9.5 | 0.0581 | 9.7 | 9.6 | 0.5630 | 9.7 | 9.5 | 0.0962 |
| . | Unadjusted Data . | Adjusted with IPW . | Propensity Score Matching . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| . | PAM . | ZA . | P-value . | PAM . | ZA . | P-value . | PAM . | ZA . | P-value . |
| Age (mean) | |||||||||
| Male Sex (%) | 98 | 96.1 | 0.0773 | 97.3 | 97.1 | 0.8304 | 96.6 | 96.6 | 1.0000 |
| Race (%) | |||||||||
| White and other | 74.5 | 70 | 72.8 | 73 | 70.5 | 71.6 | |||
| Black | 25.5 | 30 | 0.1169 | 27.2 | 27 | 0.9381 | 29.5 | 28.4 | 0.7397 |
| Mean Charlson score | 2.6 | 2.4 | 0.1851 | 2.6 | 2.5 | 0.3721 | 2.6 | 2.4 | 0.3503 |
| Transplant (%) | 15.6 | 11 | 0.0385 | 13.7 | 13.8 | 0.9591 | 11.4 | 11.4 | 1.0000 |
| Melphalan_use (%) | 35.3 | 36.8 | 0.6199 | 36.2 | 35.5 | 0.8112 | 38.4 | 36.7 | 0.6404 |
| Lenalidamide_use(%) | 21.7 | 27.4 | 0.0394 | 23.4 | 23.9 | 0.8532 | 24.7 | 27.6 | 0.3910 |
| Thalidomide_use(%) | 51.3 | 52.7 | 0.6643 | 51.5 | 51.3 | 0.9396 | 51.1 | 52.8 | 0.6508 |
| Steroid Alone (%) | 22.7 | 16.2 | 0.0125 | 20.5 | 20.8 | 0.9133 | 19.0 | 17.1 | 0.4926 |
| Bortezomib_use(%) | 34.3 | 32.9 | 0.6397 | 33.7 | 32.9 | 0.7836 | 34.1 | 33.2 | 0.8109 |
| Hemoglobin (mean) | 10.7 | 10.7 | 0.7442 | 10.8 | 10.6 | 0.1493 | 10.9 | 10.7 | 0.2788 |
| Creatinine (mean) | 1.9 | 1.8 | 0.0012 | 1.8 | 1.9 | 0.5361 | 1.5 | 1.6 | 0.7944 |
| Albumin (mean) | 3.3 | 3.3 | 0.8803 | 3.3 | 3.2 | 0.6517 | 3.3 | 3.2 | 0.6348 |
| Calcium (mean) | 9.7 | 9.5 | 0.0581 | 9.7 | 9.6 | 0.5630 | 9.7 | 9.5 | 0.0962 |
Kaplan-Meier Survival Curves
In this large, multicenter cohort study, ZA improved OS compared to PAM in patients with MM. The benefit persisted even after controlling for known patient and treatment related prognostic factors, as well as controlling for differences in baseline patient characteristics. Bisphosphonates play a key role in the treatment of MM for the prevention of MM bone disease. Evidence suggests that bisphosphonates may also have a direct anti-tumor effect in MM. Our study adds to this growing body of evidence and provides rationale for selecting ZA over PAM in most patients with MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal