Abstract
The survival of patients with multiple myeloma (MM) has considerably improved during the last decade. MM at presentation is mostly limited to the bone marrow, with circulating plasma cells seen in a modest proportion of patients. Organ infiltration or soft tissue involvement by the tumor cells is relatively uncommon at diagnosis; however, several recent reports suggest an increasing number of patients presenting with extramedullary disease at the time of relapse. This could be related to several aspects, especially increased use of more sensitive imaging studies and the newer therapies. We undertook the current study to examine the changes in incidence and potential predisposing causes for development of clinically detected EMD.
We retrospectively examined the cohort of 1,051 patients with newly diagnosed MM seen at Mayo Clinic between Jan 2001 and Dec 2010, for their initial evaluation and treatment. Data regarding baseline characteristics, site of EMD, types of therapy and response were extracted from medical records. EMD was defined as a plasmacytoma outside the bone and not contiguous to any bone lesion. Cox proportional hazards model was used to estimate the effect of variables on development of EMD.
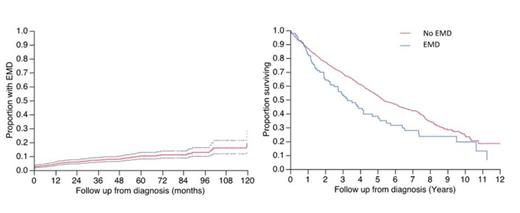
The median age at the diagnosis of MM was 66 years (range, 22-93) with 19% >75 years; 59% were male. The median estimated follow up for the entire cohort was 5.9 years, 492 (47%) were alive at the time of analysis. Over 4139 person years of follow up, 93 patients had an EMD detected (9%), including 32 patients (2.5%) in whom it was found at diagnosis. The median time to detection of EMD among the 61 patients in whom EMD developed after diagnosis, was 26 months (1 mo -10 yrs). The cumulative risk of developing EMD is shown in figure 1A and does not appear to be different between patients seen earlier (2001-2005) vs. (2006-2010), at least during the initial years. The most common sites were skin and soft tissue, lymph nodes, liver/ spleen and pleura/ peritoneum. Twelve patients had a second EMD diagnosed at a median of 5 months from the first EMD. The median OS from diagnosis of MM for the 93 patients with EMD was 3.3 years vs. 5.3 years for the rest; p<0.01. Examining the risk factors associated with development of EMD, an LDH>221 (ULN), PCLI >=3%, bone marrow plasma cell%, presence of high risk FISH abnormalities (Del 17p, t(14;16) and t (14;20) and use of SCT as part of therapy were risk factors for development of EMD. Only, a PCLI >=3 and presence of high-risk FISH increased the risk of developing EMD.
Extramedullary disease in multiple myeloma, both present at diagnosis and upon relapse, is associated with poor prognosis. While there is no clear evidence of recent increase in EMD, extended follow-up of patients seen in the recent years may alter that conclusion. Patients presenting with EMD clearly appear to have higher risk disease with more proliferative cells and high-risk cytogenetic abnormalities.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal