Abstract
PBL is a known, but uncommon Non Hodgkin's Lymphoma (NHL). The data regarding its presentation and treatment, are few, and come from single institution studies. There are no large prospective trials available. The treatment has been similar to other NHL and the role of RT not clear in the contemporary period.
We reviewed data from Surveillance, Epidemiology, and End Results (SEER) 17 Regs Research Data registry for PBL patients. Patients with extra-nodal NHL arising from the bony structures, as their primary site, were chosen for the analysis. Analysis was done using SPSS Statistics software.
Data regarding 2700 patients were available and 54% of the patients were men, rest female. The median age at presentation was 58 (range 1-85 years. These patients were diagnosed with PBL from 1973 thru 2010. Diffuse Large B Cell Lymphoma (DLBCL) was the most common subtype – 62.7% and B cell Lymphoma (NOS) was the second most common 8.9%. Staging data for the PBL was available in 54.9% of all patients and among those with data available, only 14% had stage 4 disease. RT data was available in 2638 patients (of the total 2700) and only these were included in the survival analysis. Chemotherapy data are not available from the SEER database, but given the unanimity in the treatment of aggressive lymphomas, can be presumed to be standard CHOP chemotherapy and similar across all patients.
In all, 1571 (60%) received RT. Of these, 864 patients were diagnosed before 2000 of which 612 received RT. Mean survival was higher in those who received RT 230.6 +_ S.E 6.03 vs. 200.9+- S.E 6.2 months, P=0.002. Rest of the 1774 patients were diagnosed after 2000 of which 959 received RT. Mean survival was 62.5 +- SE 1.37 months in those who received RT as compared to 56.4 +_ SE 1.5 months in those who did not receive RT, p= 0.026.
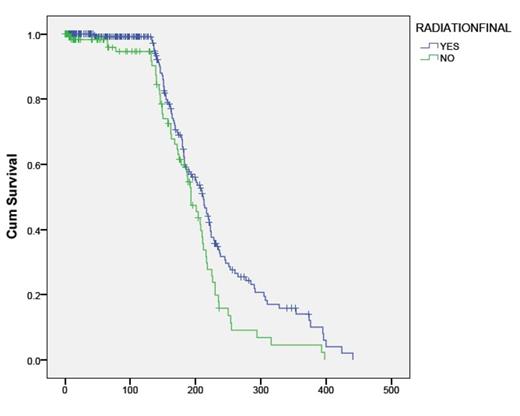
DLBCL was the pathological subtype in1654 patients, with a mean age of 58 years and 54.4 % of these patients were men. Data about staging was not available for 53% of these patients, and of those with staging data known, 14.6 % were stage 4. One thousand and eighteen patients received RT. Among patients with DLBCL, mean survival was higher in those who received RT 115.6 +_ S.E 4.09 months vs 86.8 +- S.E 3.6 months in those who did not receive RT, P=0.0001. (Figure 1, Kaplan-Meier survival curve for the two groups). We also calculated survival in the two groups after excluding stage 4 , mean survival in those who received RT 124+- S.E 4.4 was higher than those who did not receive RT 100.2 +- SE 4.3 , p=0.0001.
KM Survival curve in DLBC Lymphoma patients showing survival in months in those who received radiation therapy versus those who did not receive radiation therapy , p= 0.0001
KM Survival curve in DLBC Lymphoma patients showing survival in months in those who received radiation therapy versus those who did not receive radiation therapy , p= 0.0001
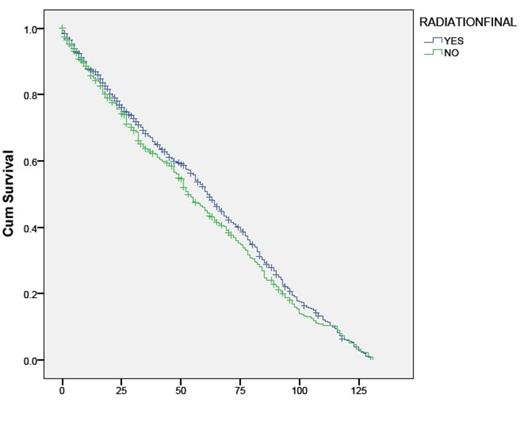
Survival among the patients with DLBCL were analyzed based on date of diagnosis and compared among patients' who were diagnosed before 2000 or during/after 2000, as the use of rituximab in addition to chemotherapy started after 2000. One thousand and thirty seven patients were diagnosed after 2000 , in these patients , mean survival was not statistically different in those who received RT (60.93+_ S.E 1.6 months )when compared to those who did not receive RT ( 57.14+- 1.9months ) , p= 0.304. (Figure 2). Rest of the 517 patients were diagnosed before 2000 of which 367 received RT. Mean survival was higher (230.7+-S.E.7.9 ) in those who received RT in this group as compared to those who did not receive RT ( 197+-8.6 ) , p=0.01 (Figure 3).
KM Survival curve in DLBC Lymphoma patients diagnosed after 2000 showing survival in months in those who received radiation therapy versus those who did not receive radiation therapy was not stastically different , p= 0.30
KM Survival curve in DLBC Lymphoma patients diagnosed after 2000 showing survival in months in those who received radiation therapy versus those who did not receive radiation therapy was not stastically different , p= 0.30
KM Survival curve in DLBC Lymphoma patients diagnosed before 2000 showing survival in months in those who received radiation therapy versus those who did not receive radiation therapy, p= 0.01
KM Survival curve in DLBC Lymphoma patients diagnosed before 2000 showing survival in months in those who received radiation therapy versus those who did not receive radiation therapy, p= 0.01
DLBCL is the most common subtype of PBL, with a good prognosis. The benefit of RT is supported in PBL as a whole group. However, in patients with DLBCL treated after 2000, there was no statistically significant improvement after addition to RT. Prospective trials using chemo-immunotherapy with rituximab are needed to assess the need for RT, as the synergistic beneficial effects of Rituximab, may have reduced the need of RT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal