Abstract
The International Prognostic Index (IPI) and the age-adjusted IPI (aaIPI) are the most commonly used tools to predict outcomes in patients with Non-Hodgkin Lymphoma (NHL). The IPI does not take into account sex or race. In the pre-rituximab era, sex was found to be a strong predictor of poor prognosis in low-grade lymphomas. While there is emerging evidence that female sex is associated with better survival in patients with diffuse large B-cell lymphoma (DLBCL) treated with R-CHOP, much less is known about the prognostic impact of race. We retrospectively assessed the impact of sex and race on overall survival in patients with indolent and aggressive NHL treated at any stage with rituximab at our institution.
We retrospectively identified all patients >/=18 years who were diagnosed with B-cell NHL (except SLL/CLL and Burkitt lymphoma) between 1/1/2000 and 12/31/2010 and received rituximab at any stage as part of their therapy at the Montefiore Medical Center. We collected data on histology, age (<60 vs. >/=60), date of diagnosis, date and status at last follow-up, and stage from the MECCC Cancer registry, and we obtained data on the Charlson Comorbidity Index (CCI) from Clinical Looking Glass® (CLG), an interactive software application developed at Montefiore Medical Center which integrates clinical and administrative datasets. The histological subtypes DLBCL and grade 3 follicular lymphoma (FL) were classified as “high-grade lymphoma” (HGL), while other types of lymphoma were termed “low-grade lymphoma” (LGL; these included marginal zone lymphoma, mantle cell lymphoma, grade 1 & 2 FL, and malignant lymphoma NOS). Self-reported race was classified as White, Black, Hispanic or “Other”. Only <2% of the patients were of “Other” racial background and therefore excluded from this analysis. The primary outcome was overall survival (OS) calculated as time from diagnosis to time of death. We used the Kaplan-Meier (KM) method to describe OS for race and sex and the log-rank test to test for significance (p<0.05). We used a Cox proportional hazard (CPH) model to assess the association of variables with OS. Except for age, race and sex, variables that were not significantly associated with OS (i.e. p-value>0.10 in the multivariate model) were excluded from the final model (backward elimination).
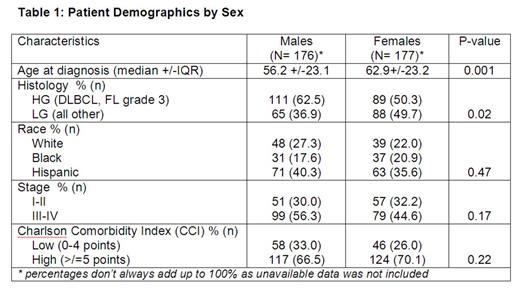
353 patients were included in the analysis. Median follow-up for all patients was 37.3 months (range 0.03-202.40). Baseline characteristics between male and females were similar with the exception of age at diagnosis and histology (see Table 1). On univariate analysis there was no OS difference between male and female patients (p=0.13), while race was associated with significant differences in OS (p=0.04; see Fig. 1). In the multivariate model, only stage >/=3 was associated with worse survival (Hazard Ratio [HR] 2.78, 95% CI 1.62-4.77; p<0.0001), but there was no significant association with OS for type of lymphoma (HGL vs. LGL) or the CCI (low vs. high score) and these 2 variables were therefore eliminated from the final multivariate model.
In the final multivariate model, female sex was associated with a 37% reduction in the risk of death (HR 0.63; 95%CI 0.40-0.98; p=0.04), while race was no longer associated with OS (Hispanic vs. White: HR 0.76, 95%CI 0.41-1.40, p=0.38; Black vs. White: HR 0.66, 95%CI 0.40-1.10; p=0.11; Black vs. Hispanic: HR 1.15; 95% CI 0.63-2.08, p=0.65).
Female patients treated at any stage with rituximab for high-grade and low-grade B-cell NHL at our institution experienced longer OS. However, we observed no racial disparity in survival in our analysis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal