Abstract
Currently recommended treatment for the primary CNS lymphoma (PCNSL) involves high-dose methotrexate (HM) preferably in combination with high-dose cytarabine (HA). However, nearly half of the patients present with locally advanced disease and poor performance status (PS) prohibiting the use of this biologically challenging therapy. On the other hand, CHOP±Rituximab with or without HM is considered suboptimal due to generaly negative, if any, published results, and a strong belief in the existence of blood-brain barrier preventing bioavailability of doxorubicin to CNS tissue. In effect, patients with DLBCL of the CNS which is the most common type of PCNSL miss the benefits of the optimal treatment for DLBCL. We evaluated the outcome of patients treated at our institution with variety of regimens evolving over time including CHOP/CHOP-like + HM, HM ± HA, and CHOP-R (rituximab) + HM. Varying proportion of patients received whole brain radiotherapy (WBRT) as well.
Between 2000 and 2011, 92 patients diagnosed with PCNSL were treated. Median age (range) was 59 (19 – 79) years, female: 55%, ECOG performance score (PS) 0-1: 30%, 2: 21%, 3-4: 49%. Most common symptoms at diagnosis were: memory loss (56%), focal symptoms (54%), confusion (36%), depression (20%), seizures (20%), agitation (13%). Diagnosis was established by stereotactic biopsy (50%), craniotomy (48%), and cerebro-spinal fluid flow cytometry in two cases. Total resection of tumor was done in 22%, tumor gross resection (debulking) in 27%, and biopsy only in 51% of patients. Cerebral / spinal parenchyma was involved in 52%, deep brain sites - in 48%. Mass effect and brain edema were present in 70% and 81%, respectively. Multiple brain lesions were present in 39% of patients. Patients were treated on 3 consecutive protocols: 2000-2006 (n=27): CHOP/CHOP-like+HM [median (range) HM total dose: 6.3 g (1.9-21)] with WBRT in 67%, 2006-2010 (n=13): HM±HA including „Bonn“ protocol [median (range) HM total dose 16.8 g (3-25.3) and median (range) HA total dose: 12 g(8-41)] with WBRT in 23%, 2009-2011 (n=19): CHOP-R + HM [median (range) HM total dose: 20 g (3-42)] with WBRT in 26% of patients. 33 patients (36%) received variety of treatments with a palliative intent.
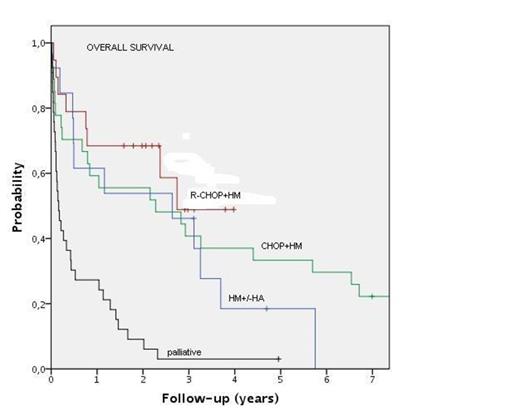
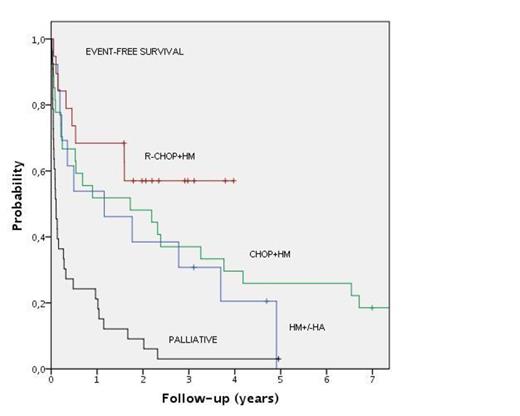
In all 92 patients, 1-, 2-, and 4-year overall survival (OS) was 50%, 41%, and 24% respectively. In patients treated with a radical approach including intended HM dose of 3 g/m2 per cycle (n=59): 1-, 2-, and 4-year OS was 63%, 59%, and 35%, respectively. In this group, event-free survival (EFS) was 58%, 49%, and 32%, respectively. In patients with PS 0-1, 2, and 3-4, 3-year OS was 67%, 26%, and 8%, respectively. 3-year EFS in these patients was 56%, 27%, and 8%, respectivly (p=0.00). Two-year OS in patients with total tumor resection, debulking, or biopsy only, was 78%, 62%, and 14%, respectively (p=0.00). Deep structure involvement vs cerebral parenchyma was not predictive of OS or EFS (p=0.33). In patients treated with CHOP/CHOP-like+HM with a median follow-up (FU) of 122 months, 1-, 2-, and 4-year OS was 59%, 55%, and 37%, and corresponding EFS was 52%, 48%, and 29%, respectively. 4 patients (15%) died of treatment-related toxicity (TRT). In patients treated with HM±HA, with a median FU of 39 months, 1-, 2-, and 4-year OS was 61%, 54%, and 18%, and corresponding EFS was 53%, 38%, and 20%, respectively. 2 patients (15%) died of TRT. In patients treated with CHOP-R+HM, with a median FU of 30 months, 1-, 2-, and 4-year OS was 68%, 68%, and 49%, and corresponding EFS was 68%, 57%, and 57%, respectively. 12 of 19 patients in this group are alive with no evidence of disease.7 patients died, 3 from disease progression, and 3 (16%) from TRT.
Outcome of PCNSL patients was highly dependent on the baseline performance score with only few patients with PS 3-4 surviving 3 years. Extent of primary surgery was also predictive of survival. In our series of 92 patients treated on consecutive clincal protocols over a period of 10 years, no benefit to methotreaxte dose escalation or addition of high-dose cytarabine could be demonstrated. The most favorable outcome was achieved with CHOP-R combined with HM at a dose of 3 g/m² per cycle.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal