Abstract
LEN (Revlimid(r)) is approved for the treatment (Tx) of transfusion-dependent anemia due to IPSS low- or intermediate-1-risk MDS associated with del(5q), with or without additional cytogenetic abnormalities (US), or with isolated del(5q) only (EU). In LEN MDS clinical trials, myelosuppression leading to neutropenia or thrombocytopenia was the leading cause of dose modifications and permanent D/C (Fenaux et al. 2011; List et al. 2006). Onset of red blood cell transfusion independence (> 56 days) occurred at a median of 4.6 weeks to LEN 10 mg (days 1-21) in MDS-004, and at a median of 4.3 weeks in MDS-003. Given 90% of pts who achieved a transfusion benefit did so by completion of 3 cycles of LEN (LEN PI, 2013), it is important to optimally manage early toxicities associated with LEN Tx to achieve best outcomes. Using the Celgene GDS database, adverse events (AEs) associated with dose modifications and early permanent D/C of LEN in MDS pts were analyzed.
The Celgene GDS database was searched for AEs spontaneously reported between Dec 27, 2005 and Jun 13, 2013 by health care practitioners and MDS pts who received LEN. A pt may be represented in the database by > 1 report. AE information could include indication, time to onset, severity and outcome of AE, and action taken with LEN. AE severity was defined as NS or serious (S; requiring hospitalization or intervention, disabling, important medical event, life threatening, or fatal). Actions taken with LEN included permanent D/C, dose modification (dose reduction or interruption) or no dose change. Incomplete AE reports were excluded from the analysis.
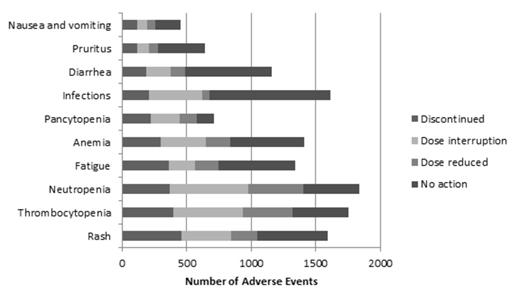
Of 42,132 pts with MDS exposed to LEN in the global post-marketing setting, 16,942 reports representing 36,793 AEs were submitted to the Celgene GDS database. The action taken with LEN was reported for the majority (73%) of AEs. The 5 most common AEs reported were neutropenia (n = 1839; 5.0%), thrombocytopenia (n = 1754; 4.8%), infections (n = 1617; 4.4%), rash (n = 1593; 4.3%), and anemia (n = 1410; 3.8%), consistent with the known safety profile of LEN (Figure). Neutropenia and thrombocytopenia were the most common AEs leading to dose modification, while, unexpectedly, rash was the most common AE leading to permanent LEN D/C. Most (91%) rash was reported as NS. Of NS rash, 26% reported permanent D/C. For all rash events, 29% (5% S vs 24% NS) reported permanent D/C, while dose modification was reported in 37% (3% S vs 34% NS) and no change in dose was reported in 34% (1% S vs 33% NS). Median time to rash onset was 9 days (range, 1-1460) for events leading to permanent D/C vs 30 days (range, 1-1825) for events leading to dose modification or no change in dose. Of the 24% permanent D/C of LEN due to NS rash, 72% permanently D/C within the first 2 cycles. Of the NS rash AEs reporting dose modifications, 76% reported an AE outcome of recovered/recovering.
Actions Taken With Top 10 Post-Marketing AEs Reporting Permanent D/C of LEN
Actions Taken With Top 10 Post-Marketing AEs Reporting Permanent D/C of LEN
Consistent with published clinical trial data, this analysis of the Celgene GDS database showed that neutropenia and thrombocytopenia were the most commonly reported AEs leading to dose modification of LEN in MDS. Unexpectedly, NS rash led to the highest rate of early permanent LEN D/C, suggesting differences in rash management in the real world vs clinical trials. The LEN label recommends permanent D/C of LEN for serious AEs (angioedema, grade [Gr] 4 rash, exfoliative or bullous rash, or if Stevens-Johnson-Syndrome or toxic epidermal necrolysis is suspected); for Gr 2-3 skin rash, dose interruption or D/C should be considered (LEN PI, 2013; SmPC, 2013). Recently, all-Gr rash was shown to be significantly associated with LEN Tx of pts with a variety of malignancies (Nardone et al. 2013). LEN-related rash in MDS has been reported in the literature to be generally self-limiting, resolving within 2-3 weeks of Tx, with NS rash being managed using antihistamines, topical steroids, or a short course of corticosteroids until rash is Gr 1 or resolved; dose interruptions for 7-14 days were suggested for Gr 3 or intolerable Gr 2 rash. LEN can generally be restarted thereafter without recurrence of rash (Giagounidis et al. 2008; Nardone et al. 2013). This analysis of Celgene GDS database showed unexpectedly that NS rash was the most common reason for early permanent D/C. NS rash should be managed by following clinical guidance with dose modification/interruption as appropriate to achieve optimal pt outcomes.
Weiss:Celgene Corporation: Employment, Equity Ownership. Gary:Celgene Corporation: Employment, Equity Ownership. Swern:Celgene: Employment, Equity Ownership. Freeman:Celgene Corporation: Employment. Sugrue:Celgene: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal