Abstract
Central venous catheters are widely used for treatments of hematologic diseases. Conventional central venous catheters (CVC), however, often cause complications such as pneumothorax, hematoma, catheter-related blood stream infection (CR-BSI), and so on. Peripherally inserted central venous Catheters (PICC) are recently expected to reduce these complications. The aim of this study was to compare the frequencies of and risk factors for complications with PICC and CVC in patients with hematologic diseases.
We retrospectively reviewed all 363 patients who had inserted PICC or CVC for treatment of hematologic diseases in January 2011 through July 2013 at the University of Tsukuba Hospital. Overall and device-specific frequencies of infectious and non-infectious complications were evaluated and potential risk factors were captured.
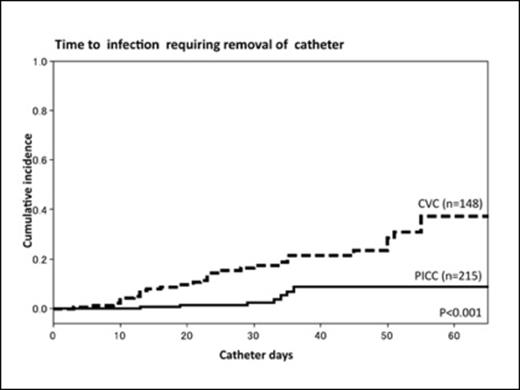
The PICC group (N = 215) and CVC group (N = 148) were similar in terms of clinical backgrounds, types of complications during catheter insertion, and total time of catheter-inserted periods. The CVC group had significantly higher proportions of patients who received hematopoietic cell transplantation (PICC 17.7% vs. CVC 49.3%, P<0.001). The significant intergroup differences were found in frequencies of CR-BSI (PICC, 1.4/1000 catheter days and CVC, 5.9/1000 catheter days; P<0.001) and local infection at the insertion site (PICC, 0.3/1000 catheter days and CVC, 2.3/1000 catheter days; P=0.002). The cumulative incidence of catheter removal for infective infectious complications was higher in the CVC group than the PICC group (PICC 8.7% vs. CVC 37.3%, P<0.001). Multivariate analysis showed that PICC significantly reduced the incidence of CR-BSI (odds ratio (OR), 0.15; 95% confidence interval (CI), 0.06-0.33; P<0.001). The incidence of CR-BSI was also significant higher in patients who received hematopoietic cell transplantation (OR, 2.4; 95%CI, 1.22-4.69; P=0.01). Phlebitis and deep vein thrombosis was noted in no patient in PICC group and 1 patient in CVC group.
Our date suggest that PICC is superior to CVC in terms of infectious complications. Low incidence of thrombophlebitis, observed in this study, is a key to a major change of practice from CVC to PICC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal