Abstract
Hospitalization is the major driver of health care utilization and costs in sickle cell disease (SCD) [Kauf et al. Am J Hematol 2009]. Allogeneic stem cell transplantation (alloSCT) is the only curative therapy available for sickle cell disease. However, it is a highly specialized, resource intense and expensive medical procedure. The objective of our study is to analyze the impact of alloSCT on the hospitalization patterns and resource utilization in children with SCD.
We used the Pediatric Health Information System (PHIS), a database of clinical and financial data from free-standing children's hospitals in the US. Using ICD-9 procedure and diagnosis codes, patients under the age of 21 who underwent alloSCT at one of the 26 PHIS hospitals from 2000-2011 were identified. We abstracted data on hospitalizations, alloSCT, resource utilization and costs. Pre and post alloSCT hospitalizations were calculated from day 0 (actual alloSCT procedure date) and does not include initial transplant hospitalization. The PHIS database provides an encrypted patient medical record number, thus we were able to follow patients over time. This allowed for a better visualization of the patient's hospitalizations trend over 11 years.
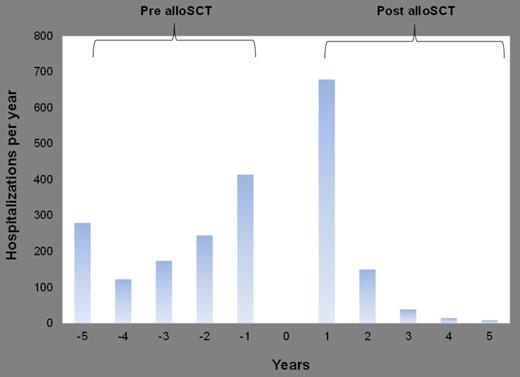
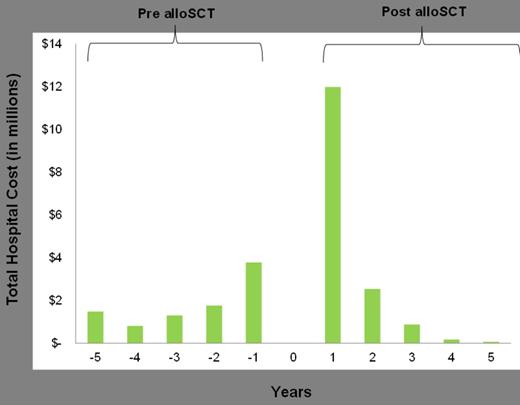
From 2000 to 2011, 186 unique pediatric patients with SCD who underwent alloSCT were identified. The median hospital length of stay (LOS) and the median total hospital charges for the initial BMT hospitalization were 38 days (31, 51) and $143,000 ($109,000, $123,000) respectively. The mean hospitalization rate was significantly higher one year after alloSCT compared to one year before the transplantation (5.8 vs. 3.1 respectively, p=0.01). However, when we expanded the analysis over 2 years, there was no significant difference in the hospitalizations between the pre and post alloSCT groups (4.8 vs. 6.8 respectively, p=0.2). Similarly, the median total hospital charges per patient were significantly higher 1 year post-alloSCT compared to one year pre-alloSCT (Table 1) whereas it was not significant when analyzed 2 years pre/post-alloSCT (Table 2). In addition, both the hospitalization rate and costs decrease consistently for several years post alloSCT suggesting a long term benefit (Figure 1A & 1B).
Patient-level summed cost (per $1000) for visits within 1 year of alloSCT
| Charges . | PRE-SCT (n=107) . | POST-SCT (n=107) . | Median Difference . | Sign-Test (p-value) . | ||||
|---|---|---|---|---|---|---|---|---|
| Median . | Min . | Max . | Median . | Min . | Max . | |||
| Clinic | 0.99 | 0.00 | 40.73 | 0.97 | 0.00 | 78.67 | -0.004 | 0.845 |
| Imaging | 0.38 | 0.00 | 13.47 | 0.42 | 0.00 | 34.60 | -0.046 | 0.320 |
| Lab | 2.66 | 0.00 | 86.47 | 6.01 | 0.00 | 249.62 | 2.265 | <.0001 |
| Other | 5.28 | 0.00 | 97.64 | 8.30 | 0.00 | 387.87 | 1.534 | 0.011 |
| Pharmacy | 1.62 | 0.00 | 63.48 | 6.52 | 0.00 | 406.39 | 3.899 | <.0001 |
| Supply | 1.08 | 0.00 | 13.73 | 0.07 | 0.00 | 74.84 | -0.074 | 0.378 |
| Total Billed | 14.61 | 0.00 | 204.07 | 23.71 | 0.75 | 1149.44 | 9.011 | 0.033 |
| Charges . | PRE-SCT (n=107) . | POST-SCT (n=107) . | Median Difference . | Sign-Test (p-value) . | ||||
|---|---|---|---|---|---|---|---|---|
| Median . | Min . | Max . | Median . | Min . | Max . | |||
| Clinic | 0.99 | 0.00 | 40.73 | 0.97 | 0.00 | 78.67 | -0.004 | 0.845 |
| Imaging | 0.38 | 0.00 | 13.47 | 0.42 | 0.00 | 34.60 | -0.046 | 0.320 |
| Lab | 2.66 | 0.00 | 86.47 | 6.01 | 0.00 | 249.62 | 2.265 | <.0001 |
| Other | 5.28 | 0.00 | 97.64 | 8.30 | 0.00 | 387.87 | 1.534 | 0.011 |
| Pharmacy | 1.62 | 0.00 | 63.48 | 6.52 | 0.00 | 406.39 | 3.899 | <.0001 |
| Supply | 1.08 | 0.00 | 13.73 | 0.07 | 0.00 | 74.84 | -0.074 | 0.378 |
| Total Billed | 14.61 | 0.00 | 204.07 | 23.71 | 0.75 | 1149.44 | 9.011 | 0.033 |
Patient-level summed cost (per $1000) for visits within two years of alloSCT
| Charges . | PRE-SCT (n=111) . | POST-SCT (n=111) . | Median Difference . | Sign-Test (p-value) . | ||||
|---|---|---|---|---|---|---|---|---|
| Median . | Min . | Max . | Median . | Min . | Max . | |||
| Clinic | 1.41 | 0.00 | 77.17 | 1.11 | 0.00 | 83.49 | -0.056 | 0.850 |
| Imaging | 0.73 | 0.00 | 25.99 | 0.66 | 0.00 | 35.18 | -0.110 | 0.101 |
| Lab | 3.84 | 0.00 | 166.29 | 6.58 | 0.00 | 261.63 | 3.035 | 0.013 |
| Other | 8.79 | 0.00 | 166.42 | 9.26 | 0.00 | 413.34 | 1.198 | 0.180 |
| Pharmacy | 2.86 | 0.00 | 66.76 | 7.62 | 0.03 | 448.85 | 4.589 | <.0001 |
| Supply | 1.39 | 0.00 | 19.77 | 0.83 | 0.00 | 78.26 | -0.223 | 0.149 |
| Total Billed | 20.12 | 0.00 | 392.49 | 27.05 | 0.75 | 1202.11 | 0.917 | 0.087 |
| Charges . | PRE-SCT (n=111) . | POST-SCT (n=111) . | Median Difference . | Sign-Test (p-value) . | ||||
|---|---|---|---|---|---|---|---|---|
| Median . | Min . | Max . | Median . | Min . | Max . | |||
| Clinic | 1.41 | 0.00 | 77.17 | 1.11 | 0.00 | 83.49 | -0.056 | 0.850 |
| Imaging | 0.73 | 0.00 | 25.99 | 0.66 | 0.00 | 35.18 | -0.110 | 0.101 |
| Lab | 3.84 | 0.00 | 166.29 | 6.58 | 0.00 | 261.63 | 3.035 | 0.013 |
| Other | 8.79 | 0.00 | 166.42 | 9.26 | 0.00 | 413.34 | 1.198 | 0.180 |
| Pharmacy | 2.86 | 0.00 | 66.76 | 7.62 | 0.03 | 448.85 | 4.589 | <.0001 |
| Supply | 1.39 | 0.00 | 19.77 | 0.83 | 0.00 | 78.26 | -0.223 | 0.149 |
| Total Billed | 20.12 | 0.00 | 392.49 | 27.05 | 0.75 | 1202.11 | 0.917 | 0.087 |
AlloSCT for SCD increases the hospitalizations and costs in the first post transplantation year. This is consistent with the previous report of increased hospitalizations in the immediate post-transplant period of alloSCT for all pediatric disorders (Shulman et al. Pediatr Blood Cancer 2013). However, over the long term, alloSCT likely improves the quality of life (by decreasing the hospitalization rate) and economic burden of pediatric sickle cell population. Further studies associating various clinical morbidities (pre & post-transplant) and healthcare utilization are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal