Abstract
Despite the existence of specific prognostic scoring systems, the International Prognostic Scoring System (IPSS) has been the most used for the evaluation of Chronic Myelomonocytic Leukemia (CMML) although it is not applicable for proliferative variants. Since its publication in 2002, the MD Anderson Prognostic Score (MDAPS) has been the most specific and powerful prognostic tool for CMML. Due to the recent emergence of CMML-specific Prognostic Scoring System (CPSS), we sought to determine its usefulness in our series and it was compared with the MDAPS to identify the index with the best capability to discriminate between high and low risk patients.
1) To assess the prognostic impact of each of the variables composing the prognostic scoring systems: MDAPS and CPSS and 2) to evaluate the discriminative ability of both scores to detect the highest risk patients.
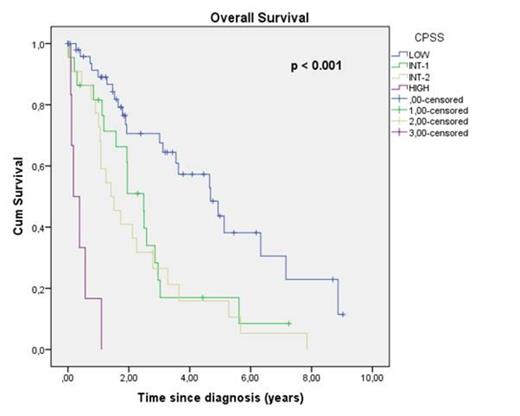
One hundred and twenty-two patients (74M/48F; median age: 76 years, 27-96 years; median follow-up: 1.88 years, 0-11.4 years) diagnosed with CMML (108 CMML-I; 14 CMML-II; 92 dysplastic CMML; 30 proliferative CMML) between 1998 and 2013 from the Hospital Clínic de Barcelona (n=110) and the Hospital Universitari Germans Trias i Pujol (n=12). The prognostic impact in terms of overall survival (OS) and leukemia free survival (LFS) of each of the variables that compose the score systems and both scores were studied by an univariate survival analysis (Kaplan-Meier; Log-Rank). The two prognostic indices were faced in a multivariate analysis (Cox Regression) to assess the discriminative power of each one to detect the highest risk patients. Finally, Receiver Operating Characteristics (ROC) curves were plotted and the area under the ROC curve was calculated as an index for the predictive value of the model.
All the variables that compose the CPSS (CMML-I vs. II, transfusion requirement, dysplastic vs. proliferative variant and CPSS cytogenetics) had prognostic impact in terms of OS (p <0.001, p <0.001, p <0.001, p =0.001) and LFS (p <0.001, p =0.005, p < 0.001, p =0.004). For the variables composing the MDAPS (Hb <120g/L, total lymphocyte count > 2500/mm3, presence of circulating immature cells and bone marrow blasts ≥ 10%) only the Hb <120g/L and the bone marrow blasts ≥ 10% impacted on OS (p =0.001, p <0.001, respectively) and only the bone marrow blasts ≥ 10% had an impact on the LFS (p <0.001). When the score systems were applied to our series, both had an impact on OS and LFS (OS CPSS p <0.001; LFS CPSS p <0.001; OS MDAPS p <0.001; LFS MDAPS p =0.037). In a multivariate analysis including gender, age, high risk patients defined by the MDAPS (high risk MDAPS) and high risk patients defined by the CPSS (high risk CPSS), only age and high risk CPSS retained its statistical significance for OS (p = 0.023, p =0.001, respectively) and only high risk CPSS for LFS (p =0.001). The greatest area under the curve (AUC), showing the highest predictive value, was observed in the mortality ROC curve of the CPSS (0.77, CI 95%: 0.68-0.86) while the AUC for the MDAPS was smaller (0.58, CI: 0.47-0.69).
In our series, CPSS seems to be a better tool than MDAPS for the prediction of OS and LFS in CMML. These data reinforce the validity of the CPSS and could serve as an additional validation cohort.
Cox Regression analysis for Overall Survial (OS)
| . | P . | HR . | 95,0% CI . | |
|---|---|---|---|---|
| Lower . | Upper . | |||
| Gender | ,396 | 1,307 | ,705 | 2,423 |
| Age | ,023 | 1,036 | 1,005 | 1,069 |
| MDAPS High Risk | ,080 | ,437 | ,173 | 1,105 |
| CPSS High Risk | ,001 | ,358 | ,194 | ,659 |
| . | P . | HR . | 95,0% CI . | |
|---|---|---|---|---|
| Lower . | Upper . | |||
| Gender | ,396 | 1,307 | ,705 | 2,423 |
| Age | ,023 | 1,036 | 1,005 | 1,069 |
| MDAPS High Risk | ,080 | ,437 | ,173 | 1,105 |
| CPSS High Risk | ,001 | ,358 | ,194 | ,659 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal