Abstract
The only curative treatment for patients with myelodysplastic syndrome (MDS) is allogeneic stem cell transplantation (allo-SCT). Decision to transplant is currently based on the International Prognostic Scoring System (IPSS), which has limitations. Recently, a revised IPSS (IPSS-R) has been developed (Blood. 2012;120:2454-2465).
To identify predictive factors for transplantation outcome, we studied 519 patients with MDS or acute myeloid leukemia (AML) evolving from MDS who received allo-SCT and were reported to the GITMO registry between 2000 and 2010.
Posttransplantation outcome according to cytogenetics. Cytogenetic abnormalities were classified according to MDS Cytogenetic Scoring System (MCSS) criteria. Four groups of patients with different overall survival (5-year OS ranging from 48% to 15%, P=.003) and probability of relapse (P=.001) after transplantation were identified. In a multivariate model, MCSS significantly affected OS (HR 1.29, P=.001) and probability of relapse (HR 1.40, P<.001). Monosomal karyotype (MK) was found in 76 patients (15%) and was associated with a dismal outcome after allo-SCT (5-year OS 10%; 5-year cumulative incidence of relapse 49%). MK maintained a significant effect on OS and probability of relapse in patients stratified according to MCSS (P<.001 and P=.001, respectively).
Posttransplantation outcome according to degree of peripheral blood cytopenia and percentage of marrow blasts. No significant effect of neutrophil and platelet count on posttransplantation outcome was noticed. The 5-year OS was 51%, 40% and 33% in patients with hemoglobin >10g/dl, between 8-10 g/dl and <8 g/dl, respectively (P=.001). The 5-year incidence of non-relapse mortality (NRM) was 29%, 37% and 44%, respectively (P=.003). The impact of hemoglobin level on posttransplantation outcome was maintained in a multivariate model (OS: HR 1.37, P=.002; NRM: HR 1.41, P=.009). Marrow blast count as stratified according to IPSS-R criteria significantly predict the probability of relapse (P=.005).
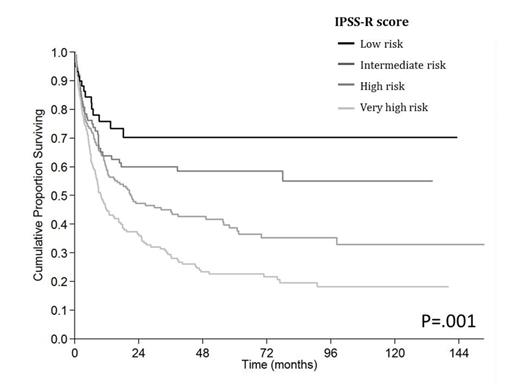
Posttransplantation outcome of patients stratified according to IPSS-R. Patients were then classified according to IPSS-R criteria: 59 patients had a low risk (11%), 89 patients (17%) an intermediate risk, 207 (40%) a high risk, and 164 (32%) a very high risk. Five-year OS was 71%, 58%, 39% and 23%, respectively (Figure 1 , P=.001). 5-year cumulative incidence of relapse was 4%, 12%, 23% and 39%, respectively (P=<.001). Compared with the IPSS-based stratification, the IPSS-R risk group would have changed for 65% of patients, 59% of which would have been assigned to a less favourable prognostic group. By applying the Akaike criterion, IPSS-R was more likely to capture prognostic information in this patient setting with respect to IPSS, especially in early stage disease (i.e., low and intermediate-1 IPSS risks).
Overall survival of MDS patients stratified according to IPSS-R criteria
We analyzed the prognostic effect of IPSS-R score by a multivariate model. The IPSS-R score significantly affected OS (HR 1.41, P<.001) and probability of relapse (HR 1.81 P<.001) in MDS patients. The effect of IPSS-R on posttransplantation outcome was maintained also when including MDS/AML as well as when stratifying patients according to type of conditioning (P form .006 to <.001).
Recipient age (≥50 years) and presence of comorbidity (high risk according to HCT-CI score) were significant risk factors for increased NRM (HR 1.79, P=.02 and HR 1.83 P=.017, respectively), while MK and lack of complete remission after induction chemotherapy showed an independent effect on relapse risk (HR 2.23, P=.001 and HR 1.94, P=.001, respectively). According to the presence of these additional risk factors, the cumulative incidence of NRM among different IPSS-R categories ranged from 13% to 52% in patients receiving standard conditioning (P<.001), and from 9% to 42% in patients receiving reduced-intensity conditioning (P<.001), while the cumulative incidence of relapse ranged from 4% to 39% (P<.001) and from 5% to 57% (P<.001), respectively.
This study clearly shows that IPSS-R allows a reliable prediction of posttransplantation outcome in MDS patients. Allo-SCT offers optimal survival benefits when the procedure is performed before MDS patients progress to advanced disease stages.
Rambaldi:Novartis: Honoraria; Sanofi: Honoraria; Italfarmaco: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal