Abstract
With the advent of tyrosine kinase inhibitors (TKIs), significant improvement has been made in the survival outcome of chronic myeloid leukemia (CML) patients. However, blastic phase (BP) CML remains a therapeutic challenge. Extramedullary disease (EMD) is a diagnostic criterion for BP, and patients with this presentation represent a unique subgroup of BP CML. The characteristics of EMD in BP CML patients have not been well described, especially in the era of TKIs.
We have analyzed CML patients with extramedullary BP either at the time of diagnosis or progressing from CP/AP from 2000 to 2011 and treated with different TKIs such as imatinib, nilotinib, dasatinib, bosutinib, and ponatinib at a single institution. All demographic, clinicopathologic variables and medication data including TKIs were collected at the time of the diagnosis of BP. Primary outcomes, overall survival (OS) were defined as time from diagnosis of BP to death.
Among a total of 284 BP CML patients, median age was 52.6 (range: 15-81) years. Males were 65.0%. 72.2% were in myeloid BP versus 27.7% in lymphoid BP. Median follow up was 1.5 (range: 0.01-12) years. Median time from diagnosis of CML to BP was 2.3 (range: 0.01-28) years. 128 (45%) patients have died. Cytogenetic analysis at diagnosis demonstrated that 34% had only Philadelphia chromosome (Ph) present while 66% had other chromosomal abnormalities besides Ph. Trisomy 8 was the most common additional chromosomal abnormality (18%). 280 (99%) were treated with TKIs. Among them, 176 (623%) were treated with TKI monotherapy, and the rest with a combination of TKI and conventional chemotherapy. Among the patients treated with TKI, 134 (48%) used imatinib; 85 (30%), dasatinib; 48 (17%), nilotinib; 7 (3%), bosutinib; and 6 (2%), ponatinib.
EMD was diagnosed in 78 patients (28%) of all BP CML patients. Patients with EMD had a median age of 52.8 (range: 19-80) while BP patients without EMD had a median age of 52.2 (range: 15-81). There were no statistically significant differences in age, gender, ethnicity, or time from diagnosis of CML to BP between EMD and non-EMD patients. Among patients with EMD 76% were myeloid, and 23% lymphoid compared with 70% myeloid and 30% lymphoid in patients without EMD (p=0.3). Patient with EMD had more Ph-only disease compared with patients without EMD (41% vs. 28%, p=0.03). Among 28 patients with deletion 7 chromosomal abnormality, only 1 patient had EMD (EMD vs. non-EMD chi-square p=0.002). There was no association between the presence of EMD and other chromosomal abnormalities such as double Ph, isochromsome 17, trisomy 8, deletion Y and variant Ph. Among patients with EMD, 39 (50%) had EMD in CNS; 22 (28%) in soft tissue, skin, or lymph nodes; 9 (12%) in bones; 8 (10%) in lung or pleura; and 4 (5%) in GI tract and liver.
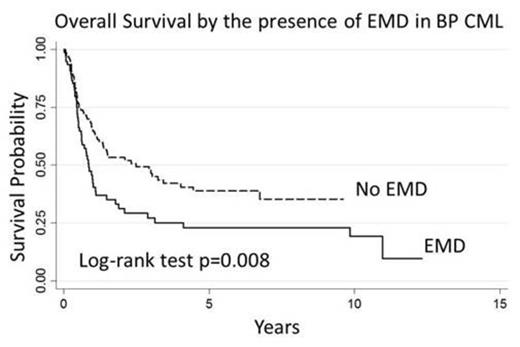
Among patient with BP CML, there were no statistically significant differences between the EMD and non-EMD groups in both complete hematologic response (CHR) rate and complete cytogenetic response (CCyR) rate at 3 months after the initiation of therapy (CHR: EMD 18% vs. non-EMD 22%, p=0.4; CCyR: EMD 8% vs. non-EMD 15%, p=0.1). However, the presence of EMD was associated with worse survival outcome (Hazard Ratio [HR]=1.62, Confidence Interval [CI]= 1.13-2.32, p=0.008). Median overall survival in patients with EMD was 0.8 versus 2.5 years in patients without EMD (log-rank test p=0.008, Figure 1). EMD in CNS was not associated with survival (HR=0.87, CI=0.50-1.51, p=0.6). In multivariate analysis controlling for age, gender, ethnicity, white cell counts, cytogenetics (presence of additional chromosomal abnormality), and pathology (myeloid versus lymphoid), EMD was still linked with adverse survival (adjusted HR=1.53, CI=1.04-2.26, p=0.03).
BP CML patients presenting with EMD are likely to have less additional chromosomal abnormality and have inferior overall survival compared with those without EMD. EMD may represent more aggressive pathophysiology in BP CML and may require more intensive treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal