Abstract
Therapy-related myeloid neoplasms (t-MN) occur as a complication after chemotherapy (CT) and/or radiation therapy (RT) and account for approximately 10 to 20% of all cases of myeloid neoplasms. t-MN often have a high prevalence of adverse-risk karyotypes. Myeloid sarcoma (MS) is a rare form of extramedullary MN with or without coexisting acute myeloid leukemia (AML). It often has similar molecular/genetic features to AML and myelodysplastic syndrome (MDS). Therapy-related MS (t-MS) is a very rare condition and has not been fully studied. We aim to investigate the features of t-MS in comparison to non-therapy-related MS.
A retrospective case review between 2003- 2013 was performed after IRB approval. Cases of MS with or without concurrent bone marrow (BM) disease were included in the study. Based on a prior history of therapy for solid or hematological cancers, patients were divided into two groups. Group 1 consisted of MS cases with a history of preceding treatment (t-MS). The remaining cases were included in Group 2. A survival analysis was performed.
A total of fifty-four MS cases were included in the study. The age ranged from 25 - 92 years (median age= 56). Male to female ratio was 1.7:1. Thirty-one cases were diagnosed as leukemia cutis, and the remaining were located in other anatomical sites. Sixteen patients had no concurrent BM disease at the time of diagnosis and 17 cases had no prior MN. Cytogenetic and/or FISH data for MS were available for 28 patients. Nineteen patients had normal cytogenetics 3 of which had abnormality via FISH (PML/RARA and MLL gene rearrangements and -7q).
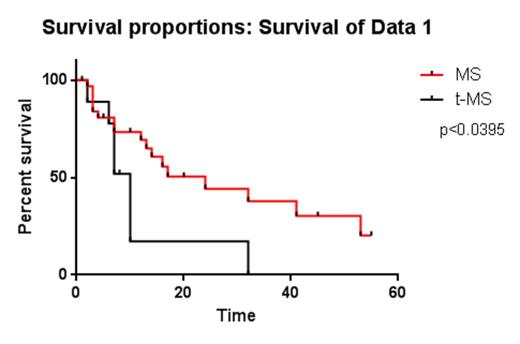
Ten of the 54 cases were found to have a prior history of CT and/or RT for solid or hematological cancers (Table 1; Group 1). Cases with prior AML history were included in group 1 (t-MS) if there was evidence of cytogenetic and/or phenotypic evolution from the original tumor. The remaining AML cases were considered relapsed or recurrent disease and included in group 2. The median age in t-MS group was 57 (39 -88 years) and M:F ratio was 1:1. In 10 cases, the most frequent prior solid malignancy was breast cancer (n=4). Five patients had a previous diagnosis of AML of a different subtype with an interval ranging 24-96 months. The overall interval time between the prior therapy and t-MS in all cases was 41 months (ranging from 6 to 126). Eight of 10 cases had no concurrent BM involvement. Molecular studies were available in 7of the 10 patients, and 3 had detectable genetic abnormalities. The treatment for both groups included intensive induction therapy with 7&3 (anthracycline/Ara-C) with or without radiotherapy and various clinical trials. Overall Survival (OS) analysis revealed a significant difference between the two groups (P-value <0.0395). The OS for t-MS patients was significantly shorter at 10 months (ranging 2 to 32; n=10) while compared to 24 months in the remaining 44 patients (1-55 months)
Group 1 (t-MS)
| . | Age . | Gender . | Prior Cancer . | Initial karyotype/FISH . | Prior Treatment . | Interval to MS (m) . | Location of MS . | Bone marrow disease . | Survival (m) . | Cytogenetics . | FISH . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 64 | M | AML | 46,XY / normal | CT+ SCT | 32 | L4 | NO | 7 | Normal | -7q |
| 2 | 39 | F | AML-MDS | N/A | CT+SCT | 63 | Ethmoid sinus | NO | 6* | Normal | Normal |
| 3 | 63 | M | AML | t(8;21) | CT | 52 | Vocal cord | NO | 32 | Normal | Normal |
| 4 | 57 | M | AML | N/A | CT+SCT | 46 | Skin | AML-MDS | 2 | N/A | N/A |
| 5 | 57 | M | AML | 46,XY | CT | 6 | Skin | AML | 10 | Trisomy, tetrasomy and pentasomy of chromosome 8 | N/A |
| 6 | 88 | M | Larynx ca | N/A | Surgery+RT | 124 | Lymph node (retroperiton) | NO | N/A | N/A | N/A |
| 7 | 51 | F | Breast ca | N/A | CT+RT | 30 | L3 | NO◊ | 29 | Normal | Normal |
| 8 | 45 | F | Breast ca | N/A | CT+RT | 23 | Skin (upper abdomen) | NO | 10 | Normal | MLL+ |
| 9 | 81 | F | Breast ca | N/A | CT | 54 | Skin (arm) | N/A | 8 | Normal | N/A |
| 10 | 43 | F | Breast ca | N/A | CT+RT | 11 | Skin (chest) | NO◊ | 7 | N/A | N/A |
| . | Age . | Gender . | Prior Cancer . | Initial karyotype/FISH . | Prior Treatment . | Interval to MS (m) . | Location of MS . | Bone marrow disease . | Survival (m) . | Cytogenetics . | FISH . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 64 | M | AML | 46,XY / normal | CT+ SCT | 32 | L4 | NO | 7 | Normal | -7q |
| 2 | 39 | F | AML-MDS | N/A | CT+SCT | 63 | Ethmoid sinus | NO | 6* | Normal | Normal |
| 3 | 63 | M | AML | t(8;21) | CT | 52 | Vocal cord | NO | 32 | Normal | Normal |
| 4 | 57 | M | AML | N/A | CT+SCT | 46 | Skin | AML-MDS | 2 | N/A | N/A |
| 5 | 57 | M | AML | 46,XY | CT | 6 | Skin | AML | 10 | Trisomy, tetrasomy and pentasomy of chromosome 8 | N/A |
| 6 | 88 | M | Larynx ca | N/A | Surgery+RT | 124 | Lymph node (retroperiton) | NO | N/A | N/A | N/A |
| 7 | 51 | F | Breast ca | N/A | CT+RT | 30 | L3 | NO◊ | 29 | Normal | Normal |
| 8 | 45 | F | Breast ca | N/A | CT+RT | 23 | Skin (upper abdomen) | NO | 10 | Normal | MLL+ |
| 9 | 81 | F | Breast ca | N/A | CT | 54 | Skin (arm) | N/A | 8 | Normal | N/A |
| 10 | 43 | F | Breast ca | N/A | CT+RT | 11 | Skin (chest) | NO◊ | 7 | N/A | N/A |
MS: Myeloid sarcoma; CT: Chemotherapy; RT: radiotherapy; SCT: stem cell transplant
Patient alive
Patient developed AML later in the course
Borate:Seattle Genetics, Inc.: Research Funding; Genoptix: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal