Abstract
A variety of factors have been investigated for their influence on outcomes post-allogeneic hematopoietic cell transplantation (HCT). Pre-HCT risk scores have been developed such as the Hematopoietic Cell Transplantation-Comorbidity Index (HCT-CI) and the modified EBMT score (mEBMT) for acute leukemias (involving age, CR status, donor type and gender mismatch). The purpose of this single-center study was to investigate the influence of these scores on outcome post-HCT in 350 patients transplanted between 1999 and 2012 for acute myeloid leukemia (AML) and to compare the predictive value of these scores.
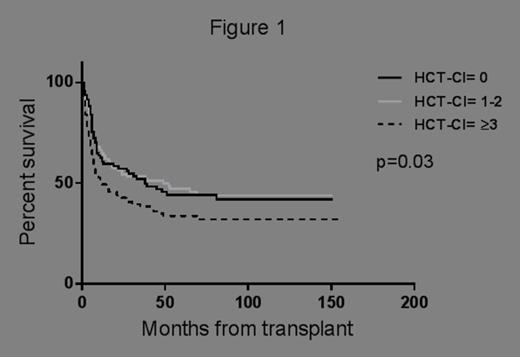
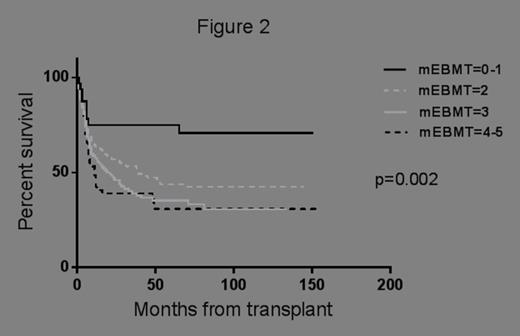
Median age of all patients at transplant was 49 years (range 18-71 years), 174 patients (50%) were female. HCT was performed in first complete remission (CR1) for 245 patients (70%) and in second complete remission (CR2) for 105 patients (30%). Cytogenetics at diagnosis were available in 289 patients (83%). Donors were matched related (n=213, 61%) or matched unrelated (n=137, 39%). Cytomegalovirus (CMV) serostatus was negative for both donor and recipient in 113 patients (32%). Peripheral blood stem cells were used as a graft source in 272 patients (78%). Myeloablative conditioning was administered to 239 (68%) patients, 111 (32%) received reduced-intensity conditioning (RIC) regimens. The HCT-CI scores were grouped as 0, 1-2 and ≥3 (94, 137 and 119 patients respectively). The mEBMT scores were grouped as 0-1, 2, 3 and 4-5 (32, 134, 120 and 64 patients respectively). Median follow-up duration among survivors was 62 months (range 12-156 months).
Multivariable analysis was performed including the HCT-CI and mEBMT scores as previously defined. Covariates already incorporated in the mEBMT score (age, CR status, related donors) were not included in the multivariable analysis. For OS, the HCT-CI score was removed from the final model due to statistical insignificance (p=0.17). However, the mEBMT score was confirmed as an independent prognostic variable for OS (p=0.00002, HR=1.5, 95%CI=1.2-1.8). For NRM, HCT-CI did not maintain significance (p=0.11) while mEBMT again was confirmed as an independent prognostic factor (p=0.0003, HR=1.5, 95%CI=1.2-1.9).
The current study showed that the mEBMT score was confirmed as an independent prognostic factor for OS and NRM in patients with AML undergoing HCT, while the HCT-CI score was not confirmed. In conclusion, the mEBMT risk score is superior to the HCT-CI score in predicting OS and NRM following allogeneic HCT in AML patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal