Abstract
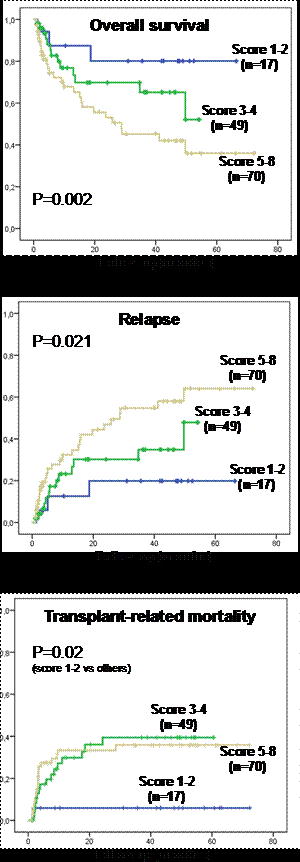
The European Group for Blood and Marrow Transplantation (EBMT) risk score provides a simple tool to assess chances and risks of hematopoietic stem cell transplantation (HSCT) for an individual patient from related and unrelated donors. To our knowledge, this score has never been applied in double umbilical cord blood transplantation (dUCBT). We recently published results of 136 patients who underwent dUCBT reported to the SFGM-TC registry from 23 centers between 2005 and 2007 (Labussiere et al., Exp. Hem. 2013). After having recorded the full data on CB units including HLA and sex, we decided to test the validity of the EBMT risk score and check its application in dUCBT. There were 88 males and 48 females with a median age of 41 years (range: 18 – 66), 76 patients with acute leukemias (42 AML, 27 ALL, 5 secondary AL and 2 Biphenotypic AL), 8 with chronic leukemias (5 lymphoid and 3 myeloid), 10 with myelodysplasic syndormes, 24 with Hodgkin and non Hodgkin lymphomas, 13 with multiple myelomas and 5 with other myeloproliferative diseases. Median interval between diagnosis and transplantation was 20.5 months (range: 3-385). At time of allogeneic transplantation, 41 patients were in first complete remission (CR1), 40 in ≥CR2 and 55 less than CR. Forty-six patients received myeloablative and 90 reduced intensity conditioning regimens. The EBMT risk score uses the 5 pre-transplant factors: age of the patient, disease status, time from diagnosis to transplant, kind of donor (related/unrelated), and donor-recipient sex combination with 0 to 1 or 2 points (pts) for each factor. Age was categorized as <20 years (0 pt; n= 6), 20 to 40 years (1 pt; n= 59) and >40 years (2 pts; n=71). For disease status we distinguished patients in CR1 at transplantation, (0 pt; n=41) from patients in CR >1 (1 pt; n=40) and patients not in CR (2 pts; n=55). Time from diagnosis to transplant was categorized into ≤12 months (0 pt; n=26) and >12 months (1pt; n=110). The adaptation of the new risk score concerned HLA and sex matching. Complete information concerning HLA typing was obtained from the database of the national network of cord blood banks on behalf of Eurocord. HLA typing was evaluated across 3 loci: HLA-A, -B and -DRB1; it was based on antigenic level for HLA-A and HLA-B, and on allelic level for HLA-DRB1. HLA matching showed patients with at least 4/6 HLA matching on HLA-A, -B and DRB1 without any mismatch on DRB1 alleles between the recipient and each UCB unit and the 2 units together (0 pt; n=77); patients with at least 4/6 HLA matching on HLA-A and -B between the recipient and each unit but without complete matching on DRB1 or with less than 4/6 HLA matching between the 2 units (1 pt; n=51), and finally patients with more than 2 mismatches on the three loci (2 pts; n=8). Donor-recipient sex combination separated all others (0 pt; n=73) from the male recipient with one female and one male cord blood unit (1pt; n=45) and male recipient with two female cord blood units (2 pts; n=18). Hence, we found 5 patients (4%) in score 1, 12 (9%) in score 2, 23 (17%) in score 3, 26 (19%) in score 4, 30 (22%) in score 5, 26 (19%) in score 6, 11 (8%) in score 7 and 3 (2%) in score 8. We pooled patients with scores 1-2; 3-4 and 5-8 as their outcomes were found to be similar. After a median follow-up of 49.5 months, the 3 years probabilities of overall and progression-free survivals for the whole population were 41% and 35% respectively. with a two-year cumulative relapse incidence of 28% (24.0 – 31.8). Interestingly patients with score 1-2 showed better overall survival rates than those with score 3-4 and 5-8 with a 3 years probability of 77%, 42% and 32% respectively (p=0.002); this was associated with a 3 years relapse incidence of 19%, 35% and 55% respectively (p=0.021), while the 3 years transplant related mortality (TRM) was 6%, 39% and 36% respectively (score 1-2 versus all others, p=0.02), Figure 1.
Figure 1
Overall survival, relapse and TRM incidences according to EBMT risk score
In conclusion, we found that the EBMT risk score can perfectly be applied to double UBCT with a significant impact on different outcomes; its use enables a better selection of patients who will benefit the more from this treatment strategy.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2013 by The American Society of Hematology
2013

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal