Abstract
Allogeneic stem cell transplantation (allo-SCT) is a potentially curative option for patients with myelodysplastic syndromes (MDS). However, allo-SCT can be associated with significant morbidity and mortality along with a risk for post-transplant disease relapse. While many MDS prognostic models exist, a prognostic model specifically designed to predict post-transplant disease relapse is yet to be developed. Therefore, we carried out this single institution study.
After due IRB approval, the Mayo Clinic MDS database (1995-2012) was retrospectively reviewed. This database contains comprehensive information on MDS clinical and pathological characteristics, treatments and SCT. Primary outcomes analyzed included disease free survival (DFS), overall survival (OS) and relapse rates at five years post allo-SCT. In addition, we evaluated transplant related mortality (TRM), non-relapse mortality (NRM), and rates of acute and chronic graft versus host disease (GVHD). DFS and OS were calculated from the time of transplantation. The prognostic relevance of several disease and transplant specific characteristics were analyzed, including: age, gender, World Health Organization (WHO) categories, therapy related MDS, cytogenetics, International Prognostic Scoring System (IPSS) and IPSS-Revised (IPSS-R) at the time of MDS diagnosis, transfusion dependence, bone marrow and circulating blast count at transplant, serum ferritin levels, SCT Co-morbidity Index, donor source, HLA matching, CMV serostatus, and conditioning regimen. Multivariate analysis was performed using the Cox Proportional Hazard Model. Survival was estimated and compared using the Kaplan Meier and Log Rank tests, respectively.
From 1995 through 2012, 96 consecutive patients with MDS underwent allo-SCT at the Mayo Clinic, Rochester. Of these, 62 were male (65%) with a median age of 54 (24-68 years). The median follow up was 31 (1-181) months. Twenty seven patients (28%) had therapy related MDS and 39 (40%) had MDS with a monosomal karyotype. IPSS-R risk stratification identified 55 (57%) patients with very high, 20 (21%) with high and 21 (22%) with intermediate/good risk disease. Fifty (52%) patients received a reduced intensity conditioning. The TRM was 8% and NRM at 5 years was 22%. Acute (grade 2 to 4) GVHD developed in 57 (59%) patients and chronic extensive GVHD was noted in 52 (54%) patients. Five-year relapse, DFS and OS rates were 24%, 42%, and 44%, respectively.
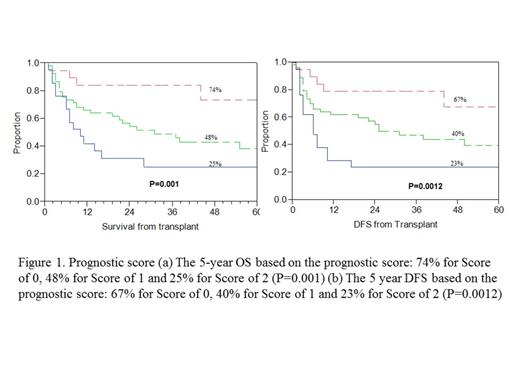
In a univariate analysis, IPSS-R (high/very high, P=0.005), therapy related MDS (P=0.009), bone marrow blast count at transplant (≥10%, P=0.01), and the presence of a monosomal karyotype (P=0.05) were significantly associated with worse DFS. On a multivariable analysis, only high or very high risk IPSS-R category (HR 7.8, P=0.005) and therapy related MDS (HR 3.9, P=0.04) retained their negative prognostic impact. Based on this finding, we developed a prognostic model that assigned one point to each of these two factors (low risk-0, intermediate-1 and high risk-2). This model successfully stratified patients based on DFS, with a 5-year DFS of 67%, 40% and 23% for low, intermediate and high risk categories respectively, P=0.0012.
This model was also successful in risk stratifying patients with regards to OS (table 1, figure 1). The presence of chronic GVHD was associated with a significantly improved DFS (62% vs 24%, P<0.0001) and OS (78% vs 19%, P<0.0001), however, as this is a post-transplant outcome, it was not included in the analysis/model.
Clinical outcomes by risk score based on our prognostic model
| Risk Score . | N . | 5 – Year Relapse Rate . | 5 – Year DFS . | 5 – Year OS . | Median OS (months) . |
|---|---|---|---|---|---|
| 0 | 22 | 5% | 67% | 74% | NR |
| 1 | 53 | 21% | 40% | 48% | 31 |
| 2 | 21 | 47% | 23% | 25% | 10 |
| P-value | 96 | <0.001 | 0.0012 | 0.001 | 0.001 |
| Risk Score . | N . | 5 – Year Relapse Rate . | 5 – Year DFS . | 5 – Year OS . | Median OS (months) . |
|---|---|---|---|---|---|
| 0 | 22 | 5% | 67% | 74% | NR |
| 1 | 53 | 21% | 40% | 48% | 31 |
| 2 | 21 | 47% | 23% | 25% | 10 |
| P-value | 96 | <0.001 | 0.0012 | 0.001 | 0.001 |
* One point is assigned to each of therapy related MDS and high or very high IPSS-R at diagnosis. DFS=disease free survival, OS=overall survival
Although the IPSS-R has not been validated in therapy related MDS or in patients who have received MDS directed therapy, the high/very high risk categories along with therapy related MDS, serve as independent predictors of OS and disease relapse after allo-SCT. Using these two variables, our prognostic model efficiently stratified patients with regards to DFS, relapse rates, and OS. Given the smaller sample size validation in a larger patient cohort will be needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal