Abstract

New drugs have significantly improved the outcome of MM patients (pts) increasing both progression free survival (PFS) and overall survival (OS). Among new drugs lenalidomide (LEN) due to its oral availability and favourable toxicity profile is an attractive option both as an induction and as a maintenance treatment, with different studies demonstrating its effectiveness. Long term therapy with LEN, however, has been associated with an increased risk of developing SPMs.
We are conducting a large phase III study to evaluate the use of LEN as induction and/or as maintenance therapy. The primary end points of the study are OS and PFS. Secondary end points are response and toxicity.
Pts are treated following an intensive or a non intensive pathway based on their eligibility for high dose Melphalan (HDM) and stem cell transplantation (ASCT) and are randomised to receive induction therapy with cyclophosphamide and dexamethasone combined with either LEN (CRD) or thalidomide (CTD). Pts failing to achieve an optimal response are randomised to receive additional therapy with cyclophosphamide, dexamethasone and bortezomib (CVD) or no extra therapy. Pts with minimal or no response will automatically receive further therapy with CVD. A randomisation between LEN maintenance and no maintenance is also performed. Data on the occurrence of SPMs are being routinely collected as part of safety assessment during all protocol phases and follow up. Analyses were performed on treatment actually received.
As per cut off of the 23rd July, 2371 pts have undergone the induction randomisation, of which 2368 are eligible for the safety analysis; 794 pts entered maintenance randomisation. The median follow up is 1.36 years from initiation of the study and 1.06 years from maintenance randomisation. Localised skin cancer other than melanoma were considered as non-invasive SPMs.
At the time of the present analysis 17 SPMs have been reported with a cumulative incidence rate of 0.7% (cumulative rate of 0.6% for invasive SPMs and 0.1% for non-invasive SPMs); four additional patients, reported as having a SPM, were excluded, after central review of the data, either due to a previous history of malignancy or because of the evidence of a pre-existing tumour other than MM at the time of study entry. The median age at the time of SPMs development is 72 years (range 61-92), and the median time from trial entry to development of SPMs is 11 months (range 2.1-27.0). The most common SPMs reported were squamous cell carcinoma (4 pts, 2 invasive and 2 non invasive), breast cancer (3 pts), colon cancer (2 pts) and prostate cancer (2 pts). No haematological SPM has so far been reported. One patient, treated according to the intensive arm with LEN both as induction and maintenance, was reported as having a suspect myelodysplasia (MDS) due to anaemia and thrombocytopenia 2.7 months after entering the maintenance randomisation. No clear histological sign of MDS was found and the values improved after stopping maintenance treatment; these data fit with treatment related toxicity and not with the development of a MDS, and the patient was excluded from this analysis.
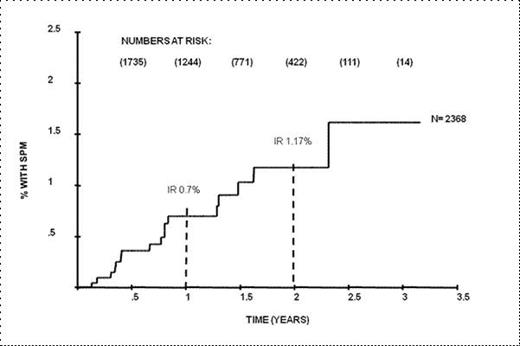
Ten out of 17 SPMs developed during maintenance treatment or follow up phase, with 7 patients having received LEN maintenance. Median time from maintenance randomisation to SPMs development is 7 months (range 2-20.6 months). The remaining 7 were diagnosed during or immediately after induction. About half of the patients (8/17) were randomised to receive LEN induction; 3 patients received LEN both as induction and as maintenance. Interestingly only one of those 3 pts had been treated according to the intensive arm. With a median follow up of 1.36 years the estimated incidence rate at 1 and 2 years are 0.70% (95% CI .40-1.22)and 1.17% (95% CI .70-1.96) respectively (Figure 1).
Our data do not confirm previous findings of an excess risk of SPMs in association with the use of LEN and HDM in presenting patients, with 12/17 pts developing SPMs treated on the non intensive pathway that does not contain HDM. Most importantly only 0.4% of the patients enrolled within the intensive pathway developed a SPM, with only 2 of them receiving LEN maintenance. Longer follow up will help to further elucidate the risk of LEN associated SPMs.
On behalf of the NCRI Haemato-Oncology subgroup
Incidence rate of SPMs
Brioli:Celgene: Honoraria. Off Label Use: The presentation include the use of Lenalidomide as induction and as maintenance treatment for newly diagnosed multiple myeloma patients. Cook:Janssen: Honoraria, Research Funding, Speakers Bureau. Cavo:Celgene: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Janssen: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Millenium: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Onyx: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Bristol-Meyer Squibb: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees. Morgan:Celgene: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Millenium: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Merck: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Johnson and Johnson: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal