Abstract

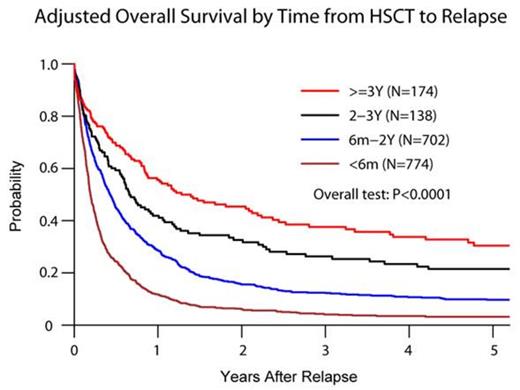
Despite the curative potential of allogeneic hematopoietic cell transplantation (alloHCT), a large number of patients with acute myeloid leukemia (AML) experience leukemia relapse after HCT. Although subsequent remissions can be achieved with salvage therapy, they are usually short lived. We evaluated survival of AML patients relapsing after alloHCT to identify prognostic factors for survival after post-transplant relapse. 1788 pediatric and adult AML CR1 & CR2 patients relapsed post-transplant (1990-2010). The median age at HCT was 30 years (yr; range, <1-76). De novo leukemia occurred in 81% and intermediate risk cytogenetics in 45%. 1374 patients (77%) underwent myeloablative (MA) and 936 patients (52%) related donor HCT. Active GVHD prior to relapse occurred in 727 subjects (41%). Median time from transplant to relapse was 7 months (mo; range, 1-177). At relapse, 357 patients (20%) received supportive care, whereas 1231 patients (69%) received intensive therapy, including chemotherapy (CT) alone (n=660), donor lymphocyte infusion (DLI)±CT (n=202; DLI+CT=51) and 2nd alloHCT±CT and/or DLI (n=369; 49% 2nd alloHCT were myeloablative). Among evaluable patients (n=846) who received intensive therapy, CR rate was 29% (n=246) [15.6% for CT alone (n=443), 37.4% for DLI±CT (n=139) and 47.3% for 2nd alloHCT±CT±DLI (n=264)]. After a median follow up of 39 mo (range, <1-193) after relapse, 229 patients (13%) survived with 5-yr overall survival of 3% (95% CI 2-5%) for patients relapsing within 6mo, 11% (95% CI 8-14%; p<0.0001 comparing to <6 mo) for 6mo-2yr, 21% (95% CI 14-28%; p<0.0001 comparing to <6 mo) for 2-3yr and 31% (95% CI 23-39%; p<0.0001 comparing to <6 mo) for ≥3yr groups. Persisting AML (n=1271, 71%) was the most common cause of death. In multivariable analysis, longer time from alloHCT to relapse (RR 0.55 6mo-2yr, 0.39 2-3yr and 0.28 ≥3yr; p<0.0001) and reduced intensity conditioning (RIC) (RR=0.77; 95% CI 0.66-0.88, p=0.0002) were associated with significantly lower mortality. In contrast, age over 40 yr (RR=1.42, 95% CI 1.24-1.64; p<0.0001), active GVHD at relapse (RR=1.25, 95% CI 1.13-1.39; p<0.0001), adverse cytogenetics (RR=1.37, 95% CI 1.09-1.71; p=0.0062), mismatched URD (RR=1.61, 95% CI 1.22-2.13; p=0.0008) or cord blood (RR=1.23, 95% CI 1.06-1.42; p=0.0078) HCT had inferior survival. We confirm poor survival of AML patients relapsing after alloHCT. Yet patients with relapse beyond 6 mo have better survival and may benefit from intensive therapy, DLI or 2nd alloHCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal