Abstract
Modern imaging techniques such as whole body multidetector CT (MDCT) and 18F-fluorodeoxyglucose-positron emission tomography CT (PET-CT) are increasingly playing an important role in the diagnosis, staging, and treatment response monitoring of patients with MM because of limitations in hematological parameters. To date, however, few studies have evaluated the roles of MDCT and PET-CT in determining clinical outcome. This study was conducted to compare these two modalities for assessment of tumor burden and prognostic relevance in patients with symptomatic MM.
Between December 2008 and November 2012, MDCT scans were performed in 64 newly diagnosed symptomatic MM patients as an initial evaluation of lytic bones and abnormal medullary and/or extramedullary lesions. Among them, PET-CT scan was performed in 56 patients. MDCT and PET-CT image acquisitions were as follows. MDCT was performed in a non-enhanced manner (acquisition time ∼45 s) and CT values (CTV) were measured using circular regions of interest for abnormal medullary lesions of the appendicular skeleton (AS; humerus and femur). The results were expressed in Hounsfield Units (HU). Since the normal CTV of yellow bone marrow ranges between -30 HU and -100 HU, we defined abnormal MDCT findings as marrow infiltration with CTV ≥ –30 HU, and the highest CTV among abnormal AS lesions was recorded in each patient. PET-CT was carried out according to the standard procedure. Data acquisition was performed in 3D mode. Field of view included the skull, upper limbs, and knees. The standardized uptake value (SUV) was calculated by the standard formula and the highest SUV (SUVmax) and SUV in the AS were collected. Visible areas of either focal or diffuse FDG uptake in bone were considered positive for myelomatous lesions. The numbers of abnormal lesions detected by these two modalities were investigated. CTV in MDCT and SUVmax in PET-CT were compared in relation to clinical variables and survival outcome. Statistical analyses were performed using STATA software ver. 12.0.
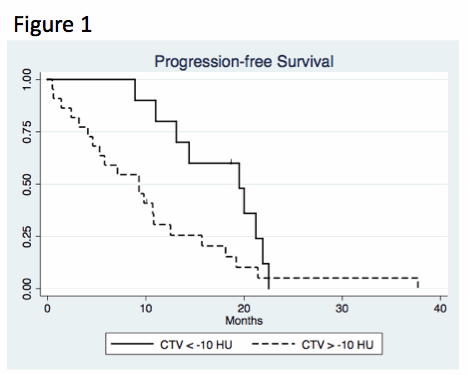
Among 64 consecutive patients (36 male and 28 female, median age 71 yr, range 44 – 90), IgG, IgA, light chain only, and non-secretory subtypes were 34, 19, 10, and 1, respectively. Fifty-one patients and 34 patients were disease stage III according to the Durie-Salmon staging system (D-S) and International Staging System (ISS), respectively. Abnormal findings of AS were detected in 53 of 64 patients (82.8%) by MDCT. However, such findings were detected only in 15 patients (26.8%) by PET-CT. Patients with D-S stage III had significantly higher CTV on MDCT than those with D-S stage I or II (mean CTV: 16.94 HU vs -9.59 HU, p = 0.032). In correlation analysis between CTV, SUVmax, serum beta-2-microglobulin, the amount of M protein, and abnormal serum lactate dehydrogenase, a positive correlation was found between CTV and M protein (r = 0.36, p = 0.003), however, SUVmax by PET-CT was not significantly correlated with any variables. All patients were treated with bortezomib and/or lenalidomide-containing regimens. Based on IMWG response criteria, the numbers of patients achieving complete remission, very good partial response, partial response, and stable disease or less were 27, 14, 20, and 3, respectively. With median follow-up duration of 18.9 months (range: 2.9 – 52.7), one-year progression-free survival (PFS) and overall survival (OS) was 46.3% and 90.2%, respectively. With the cut-off value of CTV ≥ -10 HU, high CTV had significantly shorter PFS and OS (median PFS, 9.3 months vs. 19.5 months, p = 0.041, Figure 1; median OS, not reached, p = 0.018, Figure 2). However, with the cut-off value of SUVmax ≥ 6, high SUVmax was not associated with shorter PFS or OS.
MDCT had higher sensitivity for detection of abnormal medullary lesions in AS than PET-CT. As CTVs in MDCT were significantly associated with the amount of M protein and D-S stage, CTVs may reflect tumor burden of MM. Although the follow-up duration was relatively short, our results suggest that the presence of medullary lesions in AS with high CTV may be associated with poorer outcome in patients with symptomatic MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal