Abstract
Assessment of prognosis in patients (pts) with diffuse large B cell lymphoma (DLBCL) is suboptimal. Pre-treatment clinical evaluations such as the International Prognostic Index (IPI) score are not useful in assessing response or tailoring therapy. Interim PET/CT, as an early indicator of response has a low positive predictive value and current guidelines recommend against its use, underscoring the need for improved predictive markers for early response assessment. The LymphoSIGHT™ platform is a high-throughput sequencing-based method for detecting lymphoid malignancies in peripheral blood that could potentially be used for detecting minimal residual disease (MRD) during and after treatment (Faham et al. Blood 2012). LymphoSIGHT™ has a sensitivity to detect one lymphoma cell per million leukocytes in peripheral blood and can be used to identify circulating tumor DNA in DLBCL (Armand et al., Brit J Haematol 2013). Here we assessed the ability of the sequencing method to detect lymphoma clones in pre-treatment tumor biopsy (bx) and peripheral blood samples obtained during and post-therapy from 33 DLBCL pts.
Fifty pts with DLBCL undergoing chemotherapy with curative intent were prospectively enrolled in a study to evaluate for clonal immunoglobulin (Ig) DNA in baseline tumor and peripheral blood samples collected pre-treatment, day 8, week (wk) 4, wk 7 and end of treatment. Using universal primer sets, we amplified Ig heavy chain (IGH) variable, diversity, and joining and Ig kappa chain (IGK) gene segments from genomic DNA. Amplified products were sequenced and analyzed using standardized algorithms for clonotype determination. Tumor-specific clonotypes were identified for each pt based on their high-frequency within the B-cell repertoire in the lymph node (LN) bx sample. The presence of the tumor-specific clonotype was then quantitated in plasma and serum samples obtained at pre-treatment time points. A quantitative and standardized measure of clone level per million leukocytes in each follow-up sample was determined using internal reference DNA.
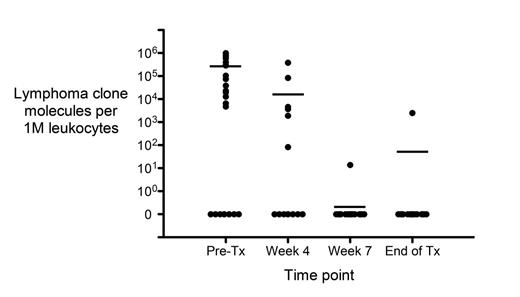
Paired tumor/plasma specimens were available from 41 pts. Of 33 LN bx samples screened, 30 had adequate DNA, and we detected a high-frequency clonal rearrangement in 25/30 (83%, CI 70-97%). In pts with an identified lymphoma specific clonotype in the bx sample, the clonotype was also detected in the plasma and/or serum compartment in 17 of 24 (71%) pts at the pre-treatment time point. We observed high qualitative and quantitative correlation (r2 = 0.89) between MRD levels measured in the matched plasma (median 0; average 53,036) and serum (median 0; average 111,496) samples. Three qualitative discordances were observed, in which the serum was negative and the plasma was positive at the same time point, all of which can be attributed to low amounts of lymphoma clone molecules that were detected in the positive samples. Pts who later relapsed tended to have higher levels of lymphoma-specific clones in their pretreatment samples compared to pts in sustained CR (t-test p=0.10).We also monitored MRD kinetics in response to therapy and observed a marked decline in MRD positivity over the course of treatment. Specifically, MRD positivity was observed in 4/5 (80%) pts at Day 8, in 6/19 (32%) at wk 4, in 1/21 (5%) at wk 7 and in 1/20 (5%) at the end of treatment (Figure 1). The average MRD level per million leukocytes was 261,681 at pre-treatment, 14,698 at wk 4, 0.35 at wk 7, and 74 at the end of treatment time point (Figure 1, horizontal lines). Thus, MRD levels demonstrated a substantial decline with treatment and reflected changes in disease load. Of note, the single pt that was MRD positive at the end of treatment was the only pt with refractory disease. Of 5/18 pts with a positive interim PET/CT following 2-3 cycles of chemotherapy, only 2 have relapsed. Three of the 5 pts (including one that relapsed) were tested for detectable clonal DNA at 7 wks, and none of the three was positive. Results of all 41 pts will be presented.
Our data demonstrate that circulating clonal tumor DNA can be detected in the blood of pts with DLBCL, and that MRD levels decline consistent with tumor burden. Further studies are warranted to better characterize the predictive value of this novel sequencing platform.
MRD levels in plasma and serum reflect changes in disease load over the course of therapy in 25 DLBCL pts.
MRD levels in plasma and serum reflect changes in disease load over the course of therapy in 25 DLBCL pts.
Weng: Sequenta, Inc: Employment, Equity Ownership. Klinger:Sequenta, Inc.: Employment, Equity Ownership. Faham:Sequenta, Inc.: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal