Abstract
Bone marrow examination is an essential and commonly performed bedside procedure in diagnosis and staging of hematological malignancies and benign hematological disorders. Although when performed on the posterior superior iliac spine(PSIS), it is considered a safe procedure with minimal complications, cases of excessive bleeding , hematoma formation, injury to neurovascular structures, retroperitoneal and intraperitoneal hemorrhage, pseudo aneurysm formation and gluteal compartment syndrome have been reported. Cases of retroperitoneal hemorrhage are presumed to occur due to penetration of the needle through the iliac crest indicating that accurate placement and angulation of the biopsy needle is critical to avoid iatrogenic complications. Bone marrow biopsy has been described in various publications and text books. However, standardized technique for positioning the biopsy needle and its penetration orientation are lacking. Various authors have described the correct needle placement and orientation as perpendicular to the bone or pointing towards the anterior superior iliac spine (ASIS) but most of the studies do not specify angulation of the needle. These methods appear to be extrapolated from personal experience and, to date, an evidence based approach for needle angulation has not been described. We present a comparison of different described approaches to perform bone marrow biopsy relative to injury to critical structures should the needle penetrate the inner bone cortex. This study compares the two most commonly used PSIS biopsy approaches that advance the needle towards: 1. The Umbilicus (Medial Approach) 2. Ipsilateral ASIS (Lateral Approach).
The study was done on cadavers in the dissection laboratory at the Albert Einstein College of Medicine. The procedure was performed by Attendings and Fellows in Hematology Division who are experienced in performing bone marrow biopsy. Manual Jamshidi needles or powered bone marrow device were used. Anatomy professors helped identify the landmarks and performed dissections after biopsy procedures. The Radiology Department assisted with performing and reading the CT scans of the pelvises.
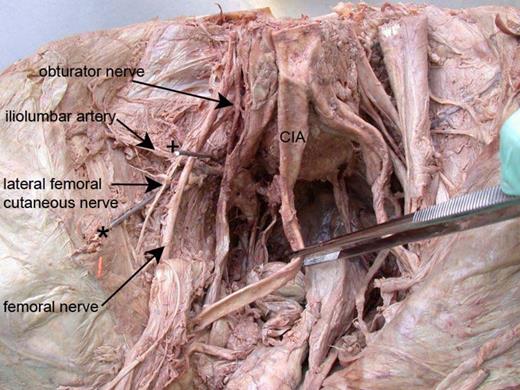
The first phase of study involved placing two dissected cadavers with intact pelvises in prone and lateral positions. Bone marrow needle was placed perpendicular to the PSIS and, during penetration, the direction was changed toward the umbilicus for the Medial Approach and towards the ASIS during the Lateral Approach. A bone marrow biopsy was obtained. Subsequently, using the same needle track, the needle was deliberately pushed through the inner ilial cortex to assess the resultant potential for injury. Keeping the needles in situ, metal wire probes were inserted via the needle for better visualization. The cadavers were further dissected to identify injury to neurovascular bundles and adjacent structures.
In the second phase, bone marrow biopsy was performed on two intact cadavers. The needles with inserted probes were left in situ to mark different angulations. The cadavers were then scanned and dissected to identify penetrated structures and closely related neurovascular bundles that were at risk had the orientation varied slightly.
Dissections and CT scan imaging showed that Lateral Approach was less likely to cause injury to significant neurovascular structures and penetrate the sacroiliac joint in comparison to the Medial Approach. Using the Medial Approach, in the event of penetration of inner cortex, we documented injury to the sacro-iliac joint, femoral nerve, common iliac vessels and mesentery of the sigmoid colon. The needle was observed in close proximity to the iliolumbar vein and artery and the lumbosacral trunk. Using the Lateral Approach, the structures adjacent to the needle were limited to the iliacus muscle and the lateral cutaneous branch of femoral nerve. The lateral approach had the added benefit of more consistent orientation since the relationship of the ASIS to the PSIS is both consistent and palpable whereas the location of the umbilicus may vary.
We suggest that the safest way to perform a bone marrow biopsy is to advance the needle in a perpendicular direction to reach the PSIS. Once the needle penetrates the outer cortex of the bone, the direction should be changed pointing towards the ipsilateral ASIS. We believe that this procedure will obviate complications reported in the literature.

No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal