Abstract
Minimal Residual Disease (MRD) status at end of first-line chemoimmunotherapy is an independent prognostic factor for patients (pts) with chronic lymphocytic leukemia (CLL). In the CLL8 trial of the German CLL Study Group, peripheral blood (PB) was monitored for MRD during follow up. Because the microenvironment is important for CLL cell growth and survival and typically it is the last site to eliminate residual disease with chemoimmunotherapy, bone marrow (BM) might be a more reliable site to monitor MRD.
Two-hundred thirty-seven pts with CLL and an indication for therapy (IWCLL-WG 2008) received first-line fludarabine, cyclophosphamide, and rituximab (FCR) on protocol between 09/2008 and 09/2012. MRD was prospectively assessed in BM and/or PB by flow cytometry using the highly sensitive international standardized approach, 2 months after the last course of treatment (final response assessment) and every 3-6 months thereafter. Kaplan-Meier estimates were compared using the log-rank test.
Sixty-one percent of pts were male, 21% were >65 years old, 40% had Rai stage III-IV, 41% had beta2-microglobulin (B2M) ≥4 mg/L, 61% had unmutated IGHV, and 21% had FISH analysis positive for deletion 11q and 7% for deletion 17p. Seventy-five percent of pts received ≥3 total courses of FCR. The complete remission (CR) and overall response (OR) rates were 65 and 97%, respectively. BM MRD negativity was achieved in 59% of pts at final response assessment.
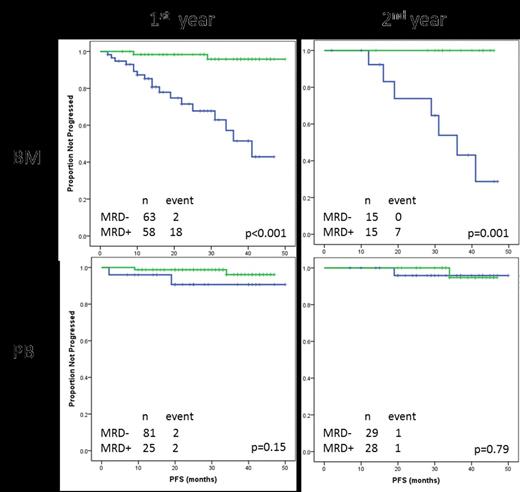
For monitoring, BM MRD was assessed in 121 pts during the 1st year and in 30 pts during the 2nd year after completion of treatment with FCR; all samples were serial. PB MRD was assessed in 106 pts during the 1st year and in 57 during the 2nd year of follow up; again all samples were serial. BM MRD negativity was observed in 63 (52%) pts during the 1st year of follow up and in 15 (50%) pts during the 2nd year. PB MRD negativity was observed at the same staging times in 81 (76%) and 29 (51%) pts, respectively. Concurrent BM and PB samples were taken during the 1st year in 51 pts, and in 6 pts during the 2nd year of follow up. We evaluated the association between MRD negativity during the 1st and 2nd year of follow-up and progression-free survival (PFS). BM MRD positive status was associated with shorter PFS when assessed during both the 1st and 2nd year of follow up (p<0.001 and p=0.001, respectively; Figure). In contrast, PB MRD positive status did not correlate with PFS for either time (p=0.15 and p=0.79, respectively; Figure).
After first-line FCR for pts with CLL, positive BM MRD may identify pts at higher risk for progression. Based on this finding, BM may be preferred to assess MRD status and pts with positive BM MRD could be considered for maintenance or consolidation strategies. Additional studies confirming these findings are warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal