Abstract
Myelodysplastic syndromes (MDS) constitute a heterogeneous group of hematopoietic stem cell disorders, characterized by ineffective hematopoiesis resulting in cytopenias and variable risk of acute myeloid leukemia (AML). To make an accurate distinction between specific risk categories in MDS, especially in low and intermediate risk MDS, a multi-diagnostic approach is recommended. To verify the efficacy of multiple diagnostic tools in MDS we used the HOVON89 study-cohort (a prospective phase II randomized multicenter study to assess the efficacy of lenalidomide with or without erythropoietin and granulocyte-colony stimulating factor in patients with low-intermediate-1 risk MDS; trial registered at www.trialregister.nl as NTR1825; EudraCT nr.: 2008-002195-10.
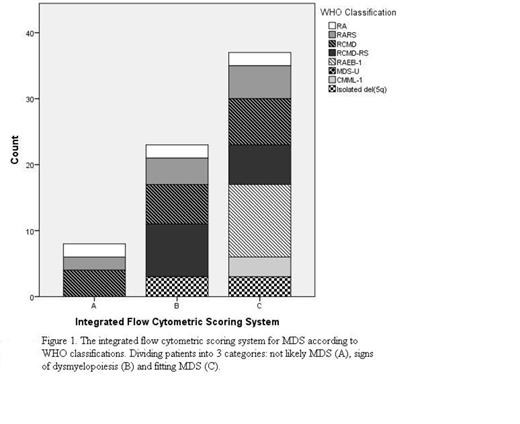
Inclusion target of the study is 200 low/intermediate-1 risk MDS patients (134 enrolled, inclusion ongoing). We collect data on cytomorphology (CM), conventional cytogenetics (CCG), fluorescence in situ hybridization (FISH) and microarray-based genomic profiling. In addition, we performed flow cytometric (FC) analysis according to European LeukemiaNet guidelines (Van de Loosdrecht et al., Haematologica 2009 and Leukemia 2012). Current CM results (N=98) identified: 8 refractory anemia (RA); 16 refractory anemia with ringed sideroblasts (RARS); 43 refractory cytopenia with multilineage dysplasia with/without ringed sideroblasts (RCMD/RCMD-RS); 16 refractory anemia with excess blast-1 (RAEB-1), 5 chronic myelomonocytic leukemia-1 (CMML-1) and 10 patients with isolated del(5q). CCG analysis (N=101) indicated 2 very good risk, 84 good risk, 13 intermediate risk and 2 poor risk patients according to the IPSS-R risk categories (Greenberg et al., Blood 2012). In addition, interphase FISH analysis (N=72) was normal in 15 patients, in 6 patients the del(5q) was confirmed. From 68 MDS patients data from both CCG and microarray were available. Microarray-based genomic profiling identified genomic abnormalities such as copy neutral loss of heterozygosity and small (<5 Mb) copy number alterations coinciding with a cancer gene in 13 patients with normal CCG. As expected in one patient the balanced translocation t(3;3)(q21;q26) was not identified by microarray-based genomic profiling.
In conclusion, this is the first prospective study in low/int-1 risk MDS that validates FC as a valuable diagnostic tool in MDS (sensitivity of FC in this cohort: 88%). FC only failed to recognize some patients with only dyserytropoiesis and dysmegakaryopoiesis by CM, not evaluated by the current scoring system. Thirteen patients with unilineage dysplasia by CM had multilineage dysplasia by FC. We postulate that RA/RARS patients with multi-lineage dysplasia by FC may have clinical features of RCMD patients and therefore a higher risk on transformation to AML. Clinical follow-up data are expected within 1.5 year.
In near future, a multi-diagnostic approach may i) identify risk categories within well defined IPSS-R subgroups, ii) predict risk on transformation and iii) select patients who might benefit from new emerging drugs for low-int-1 risk MDS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal