Abstract
MDS are a spectrum of diseases commonly divided clinically into lower- and higher-risk subtypes to reflect underlying disease biology and to guide treatment. The International Prognostic Scoring System (IPSS), the most widely used tool for risk stratification is limited in its ability to identify poor prognosis lower-risk patients (pts). A prognostic scoring system specifically for lower-risk MDS pts (LR-PSS) was developed (Garcia-Manero Leukemia 2008) based on unfavorable (non-del(5q), non–diploid) cytogenetic, hemoglobin (hgb) <10g/dl, platelet count (plt) <50 k/uL or 50-200k/uL, bone marrow blast %≥4, and age ≥60 years. The newly revised IPSS (IPSS-R) also addressed some IPSS limitations. We examined the prognostic utility of IPSS, LR-PSS and the IPSS-R in a large cohort of lower-risk MDS pts, including those with secondary (s) MDS and chronic myelomonocytic leukemia (CMML) – both excluded from IPSS and IPSS-R - within the MDS Clinical Research Consortium.
MDS pts with IPSS Score <1.5 were identified at Moffitt Cancer Center (MCC) or Cleveland Clinic (CC) from 2002-2012 and included if adequate data for analyses were available. Overall Survival (OS) was calculated from diagnosis. The Kaplan–Meier method was used to estimate median OS. Univariable analyses were performed using the log-rank test and adjusted for multiple comparisons; multivariable analyses used a Cox proportional hazards model. Harrell's c index and the Akaike information criteria (AIC) were used to assess the discriminatory power of the models and relative goodness of fit, respectively.
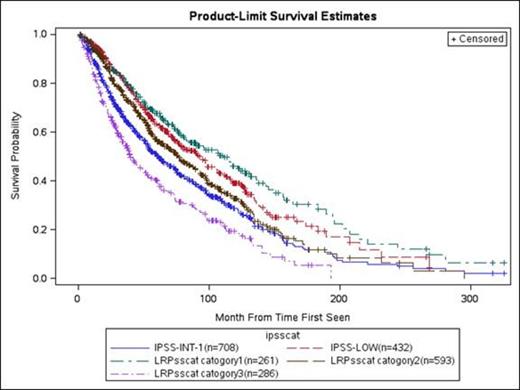
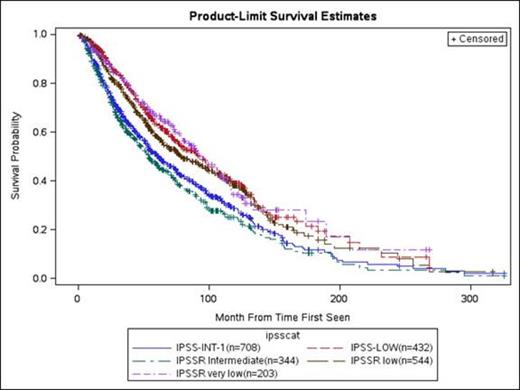
The analysis included 1196 MDS patients with IPSS scores <1.5. Comparing MCC (n=668) to CC (n=528), baseline characteristics were similar except plt <50k/uL: 16% vs. 22% (p=0.01); ANC <1.5 k/uL: 40% vs. 28% (p<0.0001); blasts <4%: 78% vs. 72% (p=0.02); sMDS: 11% vs. 6% (p=0.0024); and CMML: 2% vs. 10% (p<0.001 for WHO subgroup). R-IPSS cytogenetic groups were very good/ good/ int/ poor/ and very poor in 2/74/16/6/3 % at MCC and 2/63/19/7/10 % at CCF (p < 0.001). The median OS was 47 months (95% C.I. 44 - 52) and median follow-up of patients still alive was 62 months (range 2-326). LR-PSS and IPSS-R classifications for MCC and CCF Pts and OS are summarized in Table 1 and Figure 1. In univariable analyses, The IPSS, LR-PSS, and IPSS-R were all predictive of OS (p<0.0001 for all). Multivariable analyses confirmed the overall predictive abilities of the 3 prognostic tools adjusted for Hgb, plt, and age (p <0.0001). Compared to the IPSS-R, the LR-PSS had the higher (better) Harrell's c value (.66 vs. .60) and lower (better) AIC (5600 vs. 5605), and both were superior to the IPSS (.46 and 5609, respectively).
LR-PSS and IPSS-R Survival Estimates
| LR-PSS Category: . | MCC n(%) . | CC n(%) . | Median Survival in Months, original 2008 MD Anderson Cohort (%) . | Median Survival in Months, MCC + CC (%) . |
|---|---|---|---|---|
| 1 | 152(23) | 109(23) | 80.3 | 62.4 |
| 2 | 365(55) | 228(48) | 26.6 | 51.4 |
| 3 | 152(22) | 135(29) | 14.2 | 37.8 |
| IPSS-R Category: | Median Survival in Months, Original IPSS-R Cohort | |||
| Very Low | 120(18) | 75(16) | 81.6 | 55.4 |
| Low | 303(45) | 216(46) | 51.6 | 51.8 |
| Intermediate | 193(29) | 134(28) | 27.6 | 43.5* |
| High | 45(9) | 18 | ||
| Very High | 2(4) | 10.8 |
| LR-PSS Category: . | MCC n(%) . | CC n(%) . | Median Survival in Months, original 2008 MD Anderson Cohort (%) . | Median Survival in Months, MCC + CC (%) . |
|---|---|---|---|---|
| 1 | 152(23) | 109(23) | 80.3 | 62.4 |
| 2 | 365(55) | 228(48) | 26.6 | 51.4 |
| 3 | 152(22) | 135(29) | 14.2 | 37.8 |
| IPSS-R Category: | Median Survival in Months, Original IPSS-R Cohort | |||
| Very Low | 120(18) | 75(16) | 81.6 | 55.4 |
| Low | 303(45) | 216(46) | 51.6 | 51.8 |
| Intermediate | 193(29) | 134(28) | 27.6 | 43.5* |
| High | 45(9) | 18 | ||
| Very High | 2(4) | 10.8 |
(Combined Intermediate + High + Very High)
The LR-PSS upstaged 302 pts (25%) from IPSS low or Int-1 to LR-PSS Category 3, and downstaged 104 pts (8.6%) from Int-1 to Category 1. The IPSS-R upstaged 449 pts (37%) from IPSS low or Int-1 to IPSS-R Categories ≥Intermediate, and downstaged 18 pts (1.5% ) from Int-1 to Very Low.
The LR-PSS and IPSS-R are superior tools for distinguishing outcome among pts previously thought to have lower-risk disease by the IPSS, including those with sMDS and CMML. Upstaged pts may benefit from earlier interventions with disease-modifying therapies, and should be considered in trials targeting higher-risk MDS pts. The LR-PSS appears to provide slightly better prognostic information.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal