Abstract

Although chemotherapy induces complete remission (CR) in the majority of patients with newly diagnosed acute myeloid leukemia (AML), disease will recur in most. The pretreatment cytogenetic and molecular genetic findings are the most important predictors of outcome. However, there are some reports that post treatment parameter value are valuable for prediction of disease recurrence. Here, we examine clinical findings to assess risk of relapse in AML.
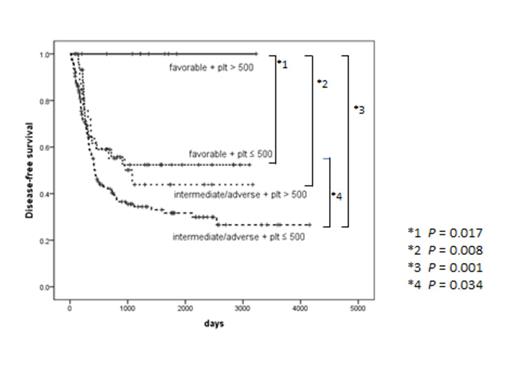
We performed a retrospective study involving 303 adult patients newly diagnosed with AML excepted acute promyelocytic leukemia between 2001 and 2012 and received either daunorubicin or idarubicin in combination with cytarabine as induction therapy. 230 patients (75.9%) obtained CR. Data was analyzed for cumulative incidence of relapse (CIR) and disease-free survival (DFS) in these 230 patients.
The study included 140 males and 90 females, with median age at diagnosis of 48 years (range, 15-77 years). Pretreatment cytogenetics was determined in 228 (99%): 57 (25%) were categorized as favorable (t(8;21) or inv(16)/t(16;16) with or without other abnormalities), 23 (10%) had abnormalities of chromosome 7 and/or complex karyotype defined as Results: One hundred and seventy three PA-AML cases, reported in 88 papers, were analyzed. AML was reported in 120 cases (69%) and APL in 53 cases (31%). The French-American-British (FAB) AML categorization, available for 59 non-M3 AML cases, showed the distribution of AML subtypes similar to that reported in non-pregnant women (M1 - 3%, M2 - 12%, M4 - 30%, M5 - 27%, M6 - 5%, M7 - 1%). Median age at diagnosis was 28 years (range 15-45). Thirty seven women (22%) were diagnosed during 1st trimester, 85 (50%) in 2nd and 47 (28%) in 3rd trimester. The trimester was not reported in 4 cases. One hundred and twenty five women received chemotherapy during pregnancy: 18 in whom therapy was started in 1st trimester, 81- in 2nd and 26 - in 3rd trimester. In 46 patients, treatment was administered either after elective abortion (n = 26), or after delivery of a live baby (n =20). Data on therapy were unavailable in 2 cases. Delay in therapy beyond 1 week (range 2-20) from diagnosis (n = 21) did not affect the overall survival (OS) compared to that obtained in women treated promptly (median 11.5 vs 10.5 months, respectively; p=0.572). Among patients for whom remission data were available (n=151), 82 (73%) treated during pregnancy, and 27 (70%) treated after delivery, achieved CR. Within a median follow-up of 9 months (range 0-300), median OS for the entire cohort was 10.5 months (9 for AML vs 15.5 for APL; p=0.001). A multivariate analysis showed APL to be the only independent predictive factor for an improved OS (p=0.037), while maternal age and treatment delay had no statistically significant impact on OS (p= 0.83 and 0.889, respectively). Notably, the OS of women with PA-AML tended to improve over time (19 months for women treated over the last 30 years vs 8 months for those treated earlier; p = 0.09) (Figure 1); however, it is still less than the median OS of 3 years reported in age-matched non-pregnant women (http://seer.cancer.gov). One hundred and forty seven pregnancies were evaluable for the fetal outcome (excluding elective abortions); 117 (80%) pregnancies ended in delivery of a live baby. Six pregnancies where fetuses were exposed to chemotherapy during the 1st (n=1) or 2nd (n=5) trimester resulted in delivery of malformed newborns; 28 pregnancies ended in fetal death (5 stillbirths, 13 intrauterine fetal deaths, 4 post-delivery deaths, 5 unplanned abortions, 1 cause unavailable). Fetal outcome was unavailable for 2 babies. The median birth weight was 2.3 Kg for the 89 babies with reported weight (range 1.7-5 Kg). Among the 83 babies for whom data about birth weight and pregnancy week were available, 59% had a weight appropriate for the gestational age, 30% were small for gestational age and 11% were large for gestational age. In 89% of cases where information was available, the delivery was pre-term. No case of fetal leukemia was reported.
Based on our retrospective analysis, the outcome of women diagnosed with AML during pregnancy appears to be worse than that reported in age-matched non-pregnant women. The survival rate of the fetuses exposed to chemotherapy is encouraging. The incidence of malformations is low and the birth weight of most newborns is appropriate for the gestational age. Therapy delay could be considered in some of these patients, but large registry-based studies are warranted to establish treatment recommendations for the management of PA-AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal