Abstract
Early response to induction therapy for AML assessed by bone marrow (BM) evaluation on day 14 (D14) post chemotherapy is considered an important predictor of achieving complete remission (CR). Our aim was to identify clinical and laboratory factors influencing the probability of CR in AML patients (pts) with positive D14 BM without receiving further chemotherapy.
Records of pts with AML treated between 1998 and 2011 were retrospectively reviewed to identify subjects with positive D14 BM who did not receive re-induction chemotherapy. The distribution of following variables such as age, white blood cell count (WBC) at the time of induction therapy, BM cellularity, percentage of blasts, disease status, and risk was compared by the univariate analysis. Recovery BM status (positive vs. negative for disease) as the response variable and age, WBC at the time of induction therapy, BM cellularity, percentage of blasts, disease status, and risk as explanatory variables were assessed by the logistic regression analysis. Poor risk AML was defined as the presence of adverse karyotype, treatment related disease or presence of antecedent hematologic disorder. Positive BM was defined as either cellularity ≥20% or ≥5% myeloblasts by IHC staining. CR was defined according to IWG 2003 criteria.
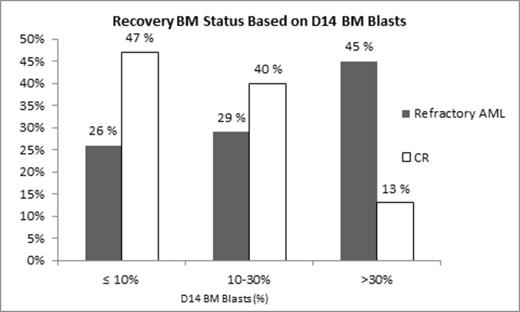
169/378 (44%) had a positive D14 BM after induction therapy and 92/169 (54%) did not receive re-induction chemotherapy. 68/92 (74%) underwent repeated BM evaluation at WBC recovery, which occurred 4-5 weeks after induction chemotherapy. Recovery BM showed refractory AML in 38/68 (56%) of cases. However, in 30/68 (44%) cases CR was achieved despite previously positive D14 BM. As demonstrated in Table 1, clinical and laboratory characteristics of the CR and refractory groups showed significant differences in the absolute percentage of D14 myeloblasts, abnormal vs. normal myeloblast phenotype, de novo vs. relapse disease status, and risk stratification. Higher blast percentage (P=.0016) was associated with significantly higher probability of having refractory AML and each 1% increase blasts on D14 BM increased the odds of refractory AML on recovery BM by 6% (OR=1.06 95% CI 1.022-1.099) (Figure 1) In contrast, no clear association between D14 BM cellularity and the recovery BM status was found. The results from the multivariate analysis were comparable with that from the univariate analysis. Blast percentage, disease status, and AML risk were strongly and jointly associated with the status of BM recovery. By using a logistic model including myeloblast percentage, myeloblast phenotype, disease status, and AML risk category we correctly predicted 31 refractory AML cases out of 38 (sensitivity = 82%) and we correctly predicted 23 CR cases out of 30 (specificity = 77%). For example, based on our formula, which incorporated blast percentage, disease status, and AML risk we estimated that in a patient with de novo, not a poor risk AML with 5% blasts on D14 BM the probability of positive recovery BM status was 6%, whereas in a patient with relapsed poor risk AML and 50% blasts on D14 BM the probability of positive recovery BM status was 98%.
| . | CR after Positive D14 BM . | Refractory AML after Positive D14 BM . | P-value . |
|---|---|---|---|
| Number | 30 | 38 | |
| Age, years | 0.17 | ||
| Median(min, max) | 55.5(20, 78) | 58(19,73) | |
| WBC at the time of induction therapy x 109/L | 0.985 | ||
| Median(min, max) | 3(0, 95) | 2.65(0, 285) | |
| BM D14 cellularity, % | 0.2 | ||
| Median(min, max) | 10 (3, 60) | 10 (5, 40) | |
| BM D14 blasts. % | 0.0028 | ||
| Median(min, max) | 11 (2, 55) | 30 (3, 85) | |
| Blast Phenotype, n | 0.0021 | ||
| Abnormal | 23 | 38 | |
| Normal | 7 | 0 | |
| Disease Status, n (%) | 0.0026 | ||
| De Novo | 25 (83%) | 18 (47%) | |
| Relapse | 5 (17%) | 20 (53%) | |
| Risk stratification, n (%) | 0.005 | ||
| Favorable | 2 (7%) | 1 (3%) | |
| Normal | 16 (53%) | 9 (24%) | |
| Poor | 12 (40%) | 28 (73%) |
| . | CR after Positive D14 BM . | Refractory AML after Positive D14 BM . | P-value . |
|---|---|---|---|
| Number | 30 | 38 | |
| Age, years | 0.17 | ||
| Median(min, max) | 55.5(20, 78) | 58(19,73) | |
| WBC at the time of induction therapy x 109/L | 0.985 | ||
| Median(min, max) | 3(0, 95) | 2.65(0, 285) | |
| BM D14 cellularity, % | 0.2 | ||
| Median(min, max) | 10 (3, 60) | 10 (5, 40) | |
| BM D14 blasts. % | 0.0028 | ||
| Median(min, max) | 11 (2, 55) | 30 (3, 85) | |
| Blast Phenotype, n | 0.0021 | ||
| Abnormal | 23 | 38 | |
| Normal | 7 | 0 | |
| Disease Status, n (%) | 0.0026 | ||
| De Novo | 25 (83%) | 18 (47%) | |
| Relapse | 5 (17%) | 20 (53%) | |
| Risk stratification, n (%) | 0.005 | ||
| Favorable | 2 (7%) | 1 (3%) | |
| Normal | 16 (53%) | 9 (24%) | |
| Poor | 12 (40%) | 28 (73%) |
Significant proportion of pts with positive D14 BM may achieve CR without subsequent chemotherapy administration. Low blast percentage, absence of phenotypically abnormal myeloblasts, de novo diagnosed AML, and absence of poor risk AML are associated with a significantly higher probability of CR. We developed a useful formula for predicting remission status in the setting of positive D14 BM that would be valuable in clinical trial protocols involving decision trees for re-induction chemotherapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal