Abstract
MYC translocations are observed in a variety of mature B-cell neoplasms and are also found in ALL. A clear assignment to an entity is not always possible in terms of immunophenotyping and morphology alone. So far, neither cytogenetics nor molecular genetics have been used to classify this group of diseases.
Analyze cytogenetic aberrations and molecular mutations in a large cohort of patients with B-cell neoplasms and MYC rearrangements to evaluate their respective value for classification.
155 patients with B-cell neoplasms harboring a MYC translocation were included in this study. Chromosome banding analysis, FISH verifying the MYC rearrangement and mutation screening of the genes ID3, MYC, TP53 and SF3B1 (only in CLL) was performed.
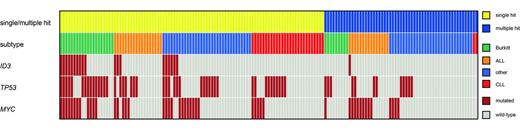
The cohort comprised 103 (66.5%) males and 52 (33.5%) females with a median age of 66.2 yrs (range: 5.5-87.1 yrs). Cytomorphologic and flow cytometric findings were heterogeneous with patients presenting as ALL (n=33, 21.3%), Burkitt lymphoma (n=29, 18.7%), CLL (n=29, 18.7%), and other mature B-cell neoplasms including follicular lymphoma, mantle cell lymphoma and PLL (n=64, 41.3%). MYC translocations occurred either as a single translocation event (“single hit”) or in addition to one, two or three other translocations involving BCL2, BCL6 and/or CCND1 (“double hit”, “triple hit” and “quadruple hit”, respectively (combined: “multiple hit”). Accordingly, the cohort was subdivided into 98/155 (63.2%) patients with single hit and 57/155 (36.8%) patients with multiple hit lymphoma (double hit: 39 (25.2%), triple hit: 16 (10.3%) and quadruple hit: 2 (1.3%)). Results of mutation analysis are depicted in the figure. TP53 mutations were identified in 57/155 (36.8%) patients and were significantly more frequent in Burkitt lymphoma compared to all other entities (18/29 (62.1%) vs. 39/126 (31.0%), p=0.003). MYC mutations were identified with a frequency of 48/155 (31.0%), without significant differences between entities. However, in patients with CLL we observed a slightly lower frequency than in all other entities (17.2% vs 34.1%, p=0.117). ID3 mutations were found in 20/155 (12.9%) cases and were significantly more frequent in Burkitt lymphoma compared to all other entities (10/29 (34.5%) vs. 10/126 (7.9%), p=0.001). Remarkably, in the subgroup of patients presenting as CLL no ID3 mutation was detected (0/29). Single hit lymphoma showed higher mutation frequencies of TP53 and ID3 compared to multiple hit lymphoma (TP53mut: 45.9% vs. 21.1%, p=0.002, ID3mut: 19.4% vs. 1.8%, p=0.001). In contrast, in single hit lymphoma the number of cytogenetic abnormalities observed in addition to MYC-translocation (ACA) was lower than in multiple hit lymphoma (mean: 3.5 vs. 8.5, p<0.001). Accordingly, cases with BCL2 rearrangements were associated with significantly lower mutation frequencies in TP53 (18.6% vs. 43.8%, p=0.005). Of note, single hit Burkitt lymphoma were characterized by significantly higher mutation frequencies of TP53, MYC and ID3 compared to Burkitt lymphoma with multiple hit (75% vs. 33.3%, p=0.048, 60% vs 11.1%, p=0.020; 50% vs 0%, p=0.011).
CLL patients were additionally analyzed for mutations in SF3B1. Interestingly, this subgroup showed a higher frequency of SF3B1 mutations compared to published data (Cazzola et al. Blood 2013,121:260-9) (11/29; 37.9% vs. 5-17%).
Correlation between single/multiple hit, subtype and molecular mutations.
1. Mutations in ID3 and TP53 were most frequently observed in cases presenting as Burkitt lymphoma and especially associated with single hit lymphoma.
2. CLL patients with MYC translocation showed a specific mutation pattern with no ID3 mutations, a low frequency of MYC mutations, but a very high frequency of SF3B1 mutations. Further, MYC translocated CLL is characterized by a low frequency of additional chromosome abnormalities and presents predominantly as single hit lymphoma.
3. Thus far, B-cell neoplasms are mainly classified based on morphological criteria and the immunophenotype. Our data suggest that the cytogenetic and molecular genetic profile might help to establish an improved classification system. The differentiation between single hit lymphoma and multiple hit lymphoma as well as the separation of the category of CLL with MYC-rearrangements is anticipated to be clinically relevant and should be further studied.
Denzel:MLL Munich Leukemia Laboratory: Employment. Kohlmann:MLL Munich Leukemia Laboratory: Employment. Roller:MLL Munich Leukemia Laboratory: Employment. Jeromin:MLL Munich Leukemia Laboratory: Employment. Alpermann:MLL Munich Leukemia Laboratory: Employment. Kienast:MLL Munich Leukemia Laboratory: Employment. Kern:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Schnittger:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal