Abstract
Allogeneic hematopoeitic cell transplantation (alloHCT) is a curative therapy for severe/very severe aplastic anemia (sAA) in adult. alloHCT from haplo-identical family donor (HD) is an alternative approach while alloHCT from matched sibling donor (MSD) is the choice of therapy. Our previous study suggested that alloHCT from matched unrelated donor (MUD) were comparable with MSD when pre-transplantation conditions were well-matched. It means poor outcome of MUD might come from poor pre-transplantation clinical factors such as delayed alloHCT. Same will be applied to HD. In this study we compared HD with alternative donors (AD; MUD or mismatched family donor) by matched case study.
We selected AD cases from KSBMT2007-01 study population who had comparable pre-transplantation clinical factors with HD by propensity-score matching. Pre-tranplatation clinical factors such as age, ATG conditioning or ABO-compatibility were matched. Therefore 48 AD cases were selected for the comparison with 16 HD cases.
Transplantation outcomes
| Clinical factors . | Alternative donors (n=48) . | Haplo-identical donors (n=16) . | P-value . |
|---|---|---|---|
| SOS | 2 (4.2%) | 0 (0%) | 1.000 |
| Acute GvHD | 19 (39.6%) | 43.8%) | 0.769 |
| Grade 3/4 | 2 (4.2%) | 2 (12.5%) | 0.258 |
| Chronic GvHD | 9 (18.8%) | 6 (37.5%) | 0.173 |
| Extensive | 4 (8.3%) | 4 (25.0%) | 0.099 |
| Engraftment failure | |||
| Neutrophil, primary | 5 (10.4%) | 2 (12.5%) | 1.000 |
| Neutrophil, secondary | 6 (12.5%) | 2 (12.5%) | 1.000 |
| Platelet | 9 (22.0%) | 5 (31.3%) | 0.505 |
| Any | 12 (25.0%) | 5 (31.3%) | 0.745 |
| Time to ANC>500/μL, days°× | 18 (15.4-20.6) | 13 (11.2-14.8) | 0.003 |
| Time to platelet>20K/μL, day°×s | 25 (21.4-28.6) | 15 (5.7-24.3) | 0.772 |
| CI of aGvHD, days°× | - | 86 (19.4-152.6) | 0.378 |
| CI of grade 3/4 aGvHD, days°× | - | - | 0.255 |
| CI of cGvHD, months°× | - | 10.4 (0-35.3) | 0.202 |
| CI of extensive cGvHD, months°× | 9.5 (5.1-13.9) | 7.3 (1.9-12.8) | 0.918 |
| Clinical factors . | Alternative donors (n=48) . | Haplo-identical donors (n=16) . | P-value . |
|---|---|---|---|
| SOS | 2 (4.2%) | 0 (0%) | 1.000 |
| Acute GvHD | 19 (39.6%) | 43.8%) | 0.769 |
| Grade 3/4 | 2 (4.2%) | 2 (12.5%) | 0.258 |
| Chronic GvHD | 9 (18.8%) | 6 (37.5%) | 0.173 |
| Extensive | 4 (8.3%) | 4 (25.0%) | 0.099 |
| Engraftment failure | |||
| Neutrophil, primary | 5 (10.4%) | 2 (12.5%) | 1.000 |
| Neutrophil, secondary | 6 (12.5%) | 2 (12.5%) | 1.000 |
| Platelet | 9 (22.0%) | 5 (31.3%) | 0.505 |
| Any | 12 (25.0%) | 5 (31.3%) | 0.745 |
| Time to ANC>500/μL, days°× | 18 (15.4-20.6) | 13 (11.2-14.8) | 0.003 |
| Time to platelet>20K/μL, day°×s | 25 (21.4-28.6) | 15 (5.7-24.3) | 0.772 |
| CI of aGvHD, days°× | - | 86 (19.4-152.6) | 0.378 |
| CI of grade 3/4 aGvHD, days°× | - | - | 0.255 |
| CI of cGvHD, months°× | - | 10.4 (0-35.3) | 0.202 |
| CI of extensive cGvHD, months°× | 9.5 (5.1-13.9) | 7.3 (1.9-12.8) | 0.918 |
°× Median (95% confidence interval), calculated by Gray's test
Abbreviations: SOS, sinusoidal obstruction syndrome; aGvHD, acute graft-versus-host disease; cGvHD, chronic graft-versus-host disease; ANC, absolute neutrophil count, CI, cumulative incidence
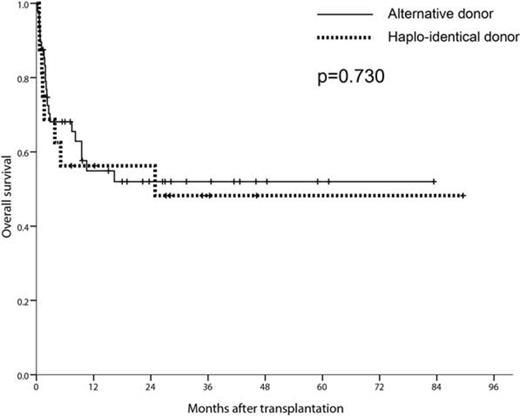
Overall survival
In conclusion, alloHCT from HD in sAA is comparable with alloHCT from AD when pre-transplantation clinical factors were similar although extensive chronic GvHD seemed frequent in HD. Therefore alloHCT from sAA could be alternative approach of alloHCT from MUD in adult sAA.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal