Abstract
The post thrombotic syndrome (PTS) is a chronic condition that develops in 20–40% of deep vein thrombosis (DVT) patients. While risk factors that predispose to the development of venous thromboembolism are widely known, factors that influence the development of PTS after DVT have not been well elucidated. Identification of factors to facilitate individualized risk assessment for PTS and thereby the need for prophylactic intervention is desirable.
We conducted a systematic review to determine whether biomarkers of fibrinolysis and endothelial dysfunction can predict the risk of developing PTS among patients diagnosed with DVT.
Studies were identified by searching the electronic databases PubMed, EMBASE, Scopus and Web of science. Studies published between January 1990 and January 2013 which measured biomarker levels in blood of adult patients with DVT, and reported rates of PTS development in these patients were included. Extracted data included source and baseline characteristics of study subjects, potential confounders that could influence the result of measured marker (e.g. malignancy, use of anticoagulants), type of biomarker, time point(s) and method of measurement, criteria for PTS diagnosis, and measure of association including adjustment variables. Risk of bias was assessed using Newcastle-Ottawa Scale, with some additional quality items specific to this literature added.
Out of 2376 records included in our primary screen of titles and abstracts, 84 articles were assessed for eligibility. Fourteen studies were included in this systematic review: 11 investigated the association between D-Dimer and PTS, three examined fibrinogen level, two measured Von Willebrand factor (VWF) antigen and activity, one study measured plasminogen activator inhibitor (PAI)-1, one assessed A Disintegrin and Metalloprotease with Thrombospondin type 1 repeats (ADAMTS)-13 antigen and activity and one study measured Factor XIII (FXIII) activity.
Studies varied with regards to inclusion and exclusion criteria (e.g. first DVT, malignancy, current anticoagulant use), use of validated scales to diagnose PTS (e.g. Villalta scale or clinical, etiological, anatomical and pathological [CEAP] classification), timing of PTS assessment, time point of biomarker measurement after DVT, measurement method, and cut off value used for analysis of association between marker and outcome.
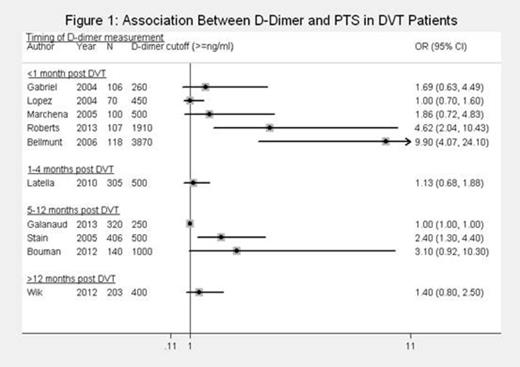
Figure 1 summarizes results from 10 studies that reported on the association between D-Dimer and PTS. We used crude Odds Ratios (OR) as the summary measure, as adjusted ORs were available for only a few studies, and adjustment variables differed between studies. Furthermore, as some studies restricted their population on certain clinical characteristics, crude ORs may already reflect a certain degree of control for confounding. In general, adjusted ORs (where available) tended to attenuate the association. Studies were grouped according to the time point of D-Dimer measurement after DVT. Even after such subgrouping, we were still unable to combine the results within subgroups due to marked clinical heterogeneity.
Three studies measured fibrinogen levels, two on the day of DVT diagnosis and one a median of 28 months after DVT. None found a significant association between fibrinogen level and the development of PTS. Similarly, no association with PTS was found in the studies examining ADAMTS-13 antigen level and activity, VWF antigen and activity, or PAI-1.
The one available study that measured FXIII activity found it to be significantly lower in patients with PTS.
We systematically reviewed the literature on the association between markers of fibrinolysis and endothelial dysfunction and the development of PTS in patients after acute DVT. An elevated D-dimer level may be an intrinsic marker of residual thrombus and/or persistent activation of clotting or inflammatory pathways that could increase the propensity to develop PTS. Similarly, impaired fibrinolysis and endothelial dysfunction are pathophysiological components of PTS. Whether these markers might be useful to predict the development of PTS after DVT is still unclear. Larger prospective studies using validated scores to diagnose PTS, strict inclusion and exclusion criteria, and accounting for confounders in the design and analysis are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal