Abstract
Ischemic cardiovascular diseases are a leading cause of mortality in the industrialized world. Cell-based therapies have been tested to promote revascularization, mainly through the release and actions of paracrine factors that may prevent apoptosis and support migration and proliferation of resident endothelial cells (EC) and circulating endothelial progenitors (EPC). The mononuclear cell fraction of umbilical cord blood (CB-MNC) is rich in pluripotent progenitors and represents an attractive cell source for therapeutic angiogenesis. In order to demonstrate the paracrine action of CB-MNC we tested the angiogenic potential of conditioned medium (CM) derived from apoptotic CB-MNC evaluating the effects exerted over mature EC and peripheral blood (PB)-derived EPC in terms of proliferation, migration and capillary-network formation in vitro.
Human Umbilical Vein Endothelial Cells (HUVEC, Lonza) were cultured in Endothelial Basal Medium (EBM2) supplemented with SingleQuotes (EGM2). EPCs were obtained from PB as “Endothelial Colony Forming Cells” (ECFC). Both HUVEC and ECFC were used for subsequent experiments from passage 2 to passage 6.
MNC were isolated from CB by density gradient centrifugation, gamma-irradiated (70Gy) to induce apoptosis and incubated in EBM2 for 72h to obtain the release of CM. CM was recovered from culture, centrifuged (4000 rpm 10 min) to remove cell debris and stored at -80°C. MNC viability after gamma-irradiation was evaluated by flow cytometry (7-AAd staining). RayBio Human Angiogenesis Array and ELISA assays (to quantify PDGF-AB, VEGF165, EGF, IGF-I) were used to assess CM soluble factors content.
The angiogenic potential of soluble factors released by gamma-irradiated MNC was assessed by Matrigel capillary-like network formation assay using the Transwell Permeable Supports and confirmed using the sole CM in the Matrigel assay. CM capacity to support HUVEC and ECFC viability was assessed by the MTT assay and the capacity to induce HUVEC and ECFC migration by the Chemicon Cell Migration Assay. EBM2 was used as control medium. All experiments were repeated at least 4 times.
Gamma-irradiation induced a significant time-dependent reduction in MNC viability (p<0.05), reaching 41±7% at 72h. The difference in viability decrease between irradiated and not irradiated MNC was statistically significant over time (p<0.001).
CM contained various cytokines and growth factors involved in the regulation of angiogenesis, wound healing, extracellular matrix remodeling and inflammation as showed by Angiogenesis Array. ELISA assays showed that irradiated MNC released an increasing amount of PDGF-AB, VEGF165 and EGF over time, while IGF-I was not detected in the CM.
Soluble factors released from irradiated MNC in the Transwell system showed a significant pro-angiogenic effect over HUVEC (p<0.001, Figure 1a) as well as over ECFC (p<0.001, Figure 1b).
Box-and-whiskers plot of Matrigel assay with irradiated MNC (a, b) and CM (c, d) over HUVEC (a, c) and ECFC (b, d)
Box-and-whiskers plot of Matrigel assay with irradiated MNC (a, b) and CM (c, d) over HUVEC (a, c) and ECFC (b, d)
Results obtained with the Matrigel Transwell system using irradiated MNC were confirmed employing CM from irradiated MNC cultured 72 hours: CM induced capillary-like network formation in both HUVEC (p<0.001, Figure 1c) and ECFC (p<0.01, Figure 1d).
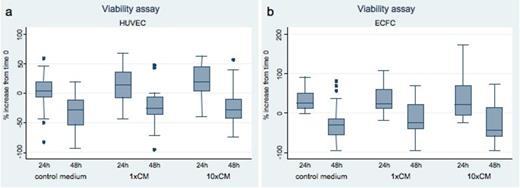
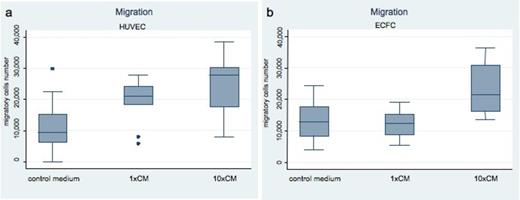
CM compared to control medium significantly increased HUVEC viability (p<0.05, Figure 2a) but not ECFC viability (Figure 2b) and significantly enhanced migration of both HUVEC (p<0.001, Figure 3a) and ECFC (p<0.001, Figure 3b).
Box-and-whiskers plot of the effect of CM over HUVEC (a) and ECFC (b) viability
Box-and-whiskers plot of the effect of CM over HUVEC (a) and ECFC (b) viability
Box-and-whiskers plot of HUVEC (a) and ECFC (b) migration toward CM
Box-and-whiskers plot of HUVEC (a) and ECFC (b) migration toward CM
Our experiments show that soluble factors released by lethally irradiated CB-MNC have an important angiogenic effect, inducing HUVEC but not ECFC proliferation, HUVEC and ECFC migration and capillary network formation in vitro. These results outline an interesting difference between mature and progenitor EC in their response to CM, which may reflect the different physiological roles that mature and progenitor EC exert during angiogenesis.
This study confirms the paracrine effect of factors released from stem cells contained in the MNC fraction, which could be exploited in regenerative medicine to induce therapeutic revascularization using CB, an easy available stem cells source.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal