Key Points
HRQoL and lifestyles of patients transplanted more than 20 years ago for thalassemia are similar to those of the general population.
Data on HRQoL in the long term provide both physicians and patients with a more complete picture of the advantages and potential risks of HSCT.
Abstract
The principal aim of our study was to investigate whether patients transplanted more than 20 years ago for β-thalassemia major had a different health-related quality of life (HRQoL) compared with the general population. The Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) and the Functional Assessment of Cancer Therapy–Bone Marrow Transplant (FACT-BMT) were received from 109 ex-thalassemia patients who underwent hematopoietic stem cell transplantation (HSCT) during the 1980s and 1990s. Adjusted comparisons were performed separately for patient age at HSCT and the presence or absence of graft-versus-host disease (GVHD). Sociodemographic and clinical variables were also analyzed. The median age of our cohort at HSCT and the time of the survey was 12 years (range, 1-36) and 34 years (range, 21-48), respectively, with a median follow-up age of 22.8 years (range, 11.7-30.3). Statistical analysis of data collected more than 20 years after HSCT showed that the long-term HRQoL of ex-thalassemia patients was very similar to that of the general population. Clinical meaningful differences were only found for the general health (GH) scale (–8.9; 95% CI, -15.0 to 2.7, P = .005). Mental health, education level, employment status, marital status, living arrangements, and birth rate were compatible with normal living patterns. The development of GVHD and older age at transplantation were important impairing factors. Additional analyses performed to evaluate HRQoL in an age-sex–matched cohort of 124 patients receiving conventional treatment of β-thalassemia revealed poorer outcomes compared with the cohort of transplanted patients.
Introduction
The past few decades have witnessed a remarkable improvement in the survival and complication-free survival rates of patients with β-thalassemia major.1,2 However, hematopoietic stem cell transplantation (HSCT) continues to be the only effective and realistic approach to curing β-thalassemia major.3 Since its first application in 1981 by the Seattle4 and Pesaro5 transplant teams, more than 3000 patients have been treated worldwide.
In recent years, the number of transplants has increased further, involving a growing number of medical centers including those of the Far and Middle East, where thalassemia is endemic and represents a serious health and socioeconomic problem.6,7 Throughout the intervening years, several new approaches have been applied to reduce the toxicity of conditioning regimens, improve strategies for the prevention of graft-versus-host disease (GVHD), and optimize supportive care. The 5-year probabilities of overall survival (OS) and thalassemia-free survival (TFS) are currently estimated as 87% to 97% and 80% to 89%, respectively.8 Successful HSCT with sustained donor engraftment and efficient hematopoiesis eliminates the need for ongoing transfusion support as well as the serious and potentially life-threatening adverse effects of iron overload. Nevertheless, complications such as growth failure, endocrinopathies, infections, cardiovascular problems, and liver disease may still occur, as well as psychological problems or the onset of secondary malignancies.9 Moreover, the posttransplantation phase may be burdened by clinical complications or adverse effects of therapy, often resulting in repeated hospital admissions, with a further impact on health-related quality of life (HRQoL).10
HRQoL is generally conceptualized as a multidimensional construct referring to patients’ perceptions of the impact of disease and treatment on their physical, psychological, and social functioning and well-being.11 Although some previous studies have investigated HRQoL issues in thalassemia patients receiving conventional treatment with blood transfusions and iron chelation,12-17 there is a paucity of evidence-based data on HRQoL after HSCT. Moreover, previous reports in this area are limited by small sample size and a relatively short follow-up ranging from 1 to 6.5 years.18-21 Other studies have investigated traditional long-term clinical outcomes, but without documenting the impact of clinical intervention on the HRQoL of patients.22,23
To our knowledge, there are no data available in the literature on long-term HRQoL of patients transplanted for β-thalassemia major. The main end point of this study was to investigate whether and to what extent HRQoL profiles of ex-thalassemia patients differed compared with their peers from the general population. A second end point was to investigate the clinical and sociodemographic features associated with HRQoL outcomes.
Material and methods
Study design and data collection
Patients eligible for this cross-sectional study were identified through the Sardinian Regional Government Health Department’s Registry. The search criteria were Sardinian TFS patients who had undergone HSCT in the 1980s and 1990s in the Centers of Pesaro and Cagliari. Overall, 130 patients were identified, 80% of whom were still living in Sardinia and 20% living in other Italian regions or abroad. All patients were initially contacted by telephone or mail to inform them of the study purposes. Respondents were sent a Survey Booklet containing survey instruments and standardized HRQoL patient questionnaires, as well as a separate questionnaire requesting basic sociodemographic and clinical information (eg, education level, employment status and type, marital status, living arrangements, children born after HSCT, and comorbidities at the time of the survey). The survey was accompanied by a letter providing clear and concise instructions on how to complete the questionnaires along with two copies of written, informed consent.
All questionnaires were delivered to the Hematology Department of the University of Cagliari at the R. Binaghi Hospital. Enrollment began in July 2011 and ended in September 2012. Further clinical data (ie, acute or chronic GVHD grading, risk classification according to Pesaro criteria) were obtained from our database.24 The study was approved by the local Ethics Committee (ASL 8 Cagliari), and written, informed consent was provided by all patients according to the Declaration of Helsinki.
Patient-reported data collection
Generic HRQoL was assessed by the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), a well-established generic HRQoL measure that is often used in cancer survivor populations.25,26 In Italy, the questionnaire was translated and adapted to the cultural context as part of the International Quality of Life Assessment project.27 The SF-36 version 1 is a 36-item questionnaire used to assess patient-reported health and functioning. This tool examines 8 domains of HRQoL: physical functioning (PF), role limitations as a result of physical functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional functioning (RE), and mental health (MH). These 8 domains can be aggregated into 2 summary measures: the physical component summary score (PCS) and the mental component summary score (MCS). The SF-36 scores obtained for our transplanted population were compared against previously published Italian population norms and adjusted for the following potential key confounders of HRQoL: age, gender, education level, comorbidity (at study entry), and marital status.28-30 We also compared the HRQoL of our cohort of transplanted patients with that of an age-sex–matched group (median age, 33; range, 18-45 years; 54% male/46% female) of 124 thalassemia patients conventionally treated with blood transfusions and iron chelation therapy in the Microcytemia Hospital of Cagliari.
Treatment-specific HRQoL was evaluated by the Functional Assessment of Cancer Therapy–Bone Marrow Transplant (FACT-BMT) scale, version 4, a self-administered tool used to assess multidimensional domains of HRQoL in patients after HSCT. It consists of the 27-item FACT-General (FACT-G) and the 23-item Bone Marrow Transplantation Subscale. The FACT-G measures 4 dimensions of QoL physical well-being (7 items), social/family well-being (7 items), emotional well-being (6 items), and functional well-being (7 items). Each item is rated on a 5-point Likert-type response scale ranging from 0 to 4, where 0 = “not at all,” 1 = “a little bit,” 2 = “somewhat,” 3 = “quite a bit,” and 4 = “very much.” Individual domain scores are summarized to give a total FACT-BMT score. Originally, the FACT-BMT scale was developed and validated in English, and thus used in several clinical trials.31,32 Later, it was translated into several other languages, including Italian.33
Statistical analysis
HRQoL outcomes were compared with those of matched peers from the Italian SF-36 normative database.28 Propensity score-matching was implemented to minimize possible bias, selecting the best possible case-control pairs given the available data. This approach has already been applied in previous studies of HRQoL.34 The prematching control group consisted of 1756 Italian adults. Age and gender were used as matching covariates, and all comparisons of HRQoL were further adjusted for age, gender, marital status, education level, and comorbidity. In addition, adjusted comparisons with matched peers were performed separately for patient age at HSCT (<15 and ≥15 years) and the presence or absence of GVHD (“yes” and “no”). Fifteen years was defined as the cutoff age between pediatric and adult patients, as reported in the published literature.18 Statistical tests evaluating significance of adjusted mean differences of the 8 SF-36 scales were Bonferroni-corrected (α = 0.00625) for multiple comparisons. Eight points on these scales were considered to be a minimally important difference (MID),35 whereas a difference of 2 points was judged as a MID for the PCS and MCS scores.36 A score difference at least equal to a MID was considered a clinically meaningful difference. FACT-BMT data were analyzed by multivariate analysis, where gender, education level, living arrangements, GVHD, and comorbidity were considered as independent variables. The association of sociodemographic and clinical variables with SF-36 and FACT-BMT outcomes was investigated by Wilcoxon and Kruskall-Wallis tests, Spearman correlations, and univariate regression analysis (α = 0.05).
Results
One-hundred nine of the 130 TFS patients (83.8%) returned the survey. Sociodemographic and clinical features of the analyzed cohort are shown in Table 1. The median age was 12 years (range, 1-36) at the time of HSCT and 34 years (range, 21-48) at enrollment. Median follow-up after HSCT was 22.8 years (range, 11.7-30.3). All patients underwent HSCT from a human leukocyte antigen–identical sibling donor during the period from July 1982 to May 1998. Of 109 patients examined, 26 were assigned to low-risk class 1, 45 to intermediate-risk class 2, and 38 to high-risk class 3.24 All patients received a myeloablative conditioning regimen based on busulfan, followed by cyclophosphamide. The GVHD prophylactic regimen mainly consisted of cyclosporine A, steroids, and/or short-course methotrexate. The incidence of acute GVHD (grade II-IV) was 35.8% (grade III-IV in 10.3% of patients); chronic GVHD affected 18.3% of the patients, but in most (65%) it was identified as limited disease. Most patients (74.3%) reported the presence of at least 1 comorbidity at the time of study inclusion: metabolic or endocrine alterations such as osteoporosis, impairment of thyroid function, major fertility issues, amenorrhea, liver disease (hepatitis C virus [HCV] infection), or minor cardiovascular problems (essential hypertension). Two patients reported a solid organ transplant after HSCT: one kidney transplant for chronic renal failure and the other a liver transplant after hepatic failure secondary to HCV-induced cirrhosis. Four patients (4.9%) reported a secondary malignancy (liver, thyroid, and tongue carcinoma, and one case of non-Hodgkin lymphoma). Seven pregnancies were reported by 6 of the 44 female patients (13.6%); 16 pregnancies regarded the partners of 11/65 male patients (16.9%). All mothers had been transplanted during the pediatric age range (<15 years), whereas the fathers had a mean age of 15 years (range, 4-26) at the time of HSCT.
Sociodemographic and clinical characteristics of 109 patients transplanted for thalassemia
| Median age at survey (range) | 34 (21-48) | Median age at HSCT (range) | 12 (1-36) |
| Gender, n (%) | Pesaro class of risk at the time of HSCT, n (%) | ||
| Male | 65 (59.7) | 1 | 26 (23.9) |
| Female | 44 (40.3) | 2 | 45 (41.3) |
| 3 | 38 (34.5) | ||
| Schooling after transplantation, n (%) | |||
| Resumed | 28 (25.7) | Follow up, median years after HSCT (range) | 22.8 (11.7-30.3) |
| Completed | 58 (48.7) | ||
| Given up | 23 (25.6) | Acute GvHD (I-IV), n (%) | 39 (35.8) |
| Grade I-II | 35 (89.7) | ||
| Education level, n (%) | Grade III-IV | 4 (10.3) | |
| Compulsory school | 28 (25.7) | ||
| High school | 61 (56) | Chronic GvHD, n (%) | 20 (18.3) |
| University degree or higher | 20 (18.3) | Limited | 13 (65) |
| Extensive | 7 (35) | ||
| Employment status, n (%) | |||
| Unemployed | 19 (17.4) | Comorbidity, n (%) | |
| Employed | 84 (77.1) | Total | 81 (74.3) |
| Inactive* | 6 (5.5) | Metabolic or endocrine | 34 (42.0) |
| Hepatic | 32 (39.5) | ||
| Type of work, n (%) | Cardiac | 27 (33.3) | |
| Full-time employment | 30 (27.6) | Gastrointestinal | 6 (7.4) |
| Part-time employment | 9 (8.3) | Neurologic | 6 (7.4) |
| Self-employed/other | 43 (39.5) | Renal | 5 (6.2) |
| Housewife | 2 (1.8) | Cutaneous | 5 (6.2) |
| Infective | 3 (3.7) | ||
| Marital status, n (%) | Pulmonary | 2 (2.5) | |
| Single | 60 (55) | Solid organ transplant after HSCT | 2 (2.5) |
| Married/Living with partner | 49 (45) | Secondary malignancy | 4 (4.9) |
| Living arrangements, n (%) | Children after HSCT, n (%) | ||
| Living alone | 15 (13.8) | Yes | 17 (15.6%) |
| Living with parents or other relatives | 45 (41.3) | No | 92 (84.4%) |
| Living with spouse/partner | 49 (44.9) | ||
| No. of total healthy births | 23 | ||
| Median age at survey (range) | 34 (21-48) | Median age at HSCT (range) | 12 (1-36) |
| Gender, n (%) | Pesaro class of risk at the time of HSCT, n (%) | ||
| Male | 65 (59.7) | 1 | 26 (23.9) |
| Female | 44 (40.3) | 2 | 45 (41.3) |
| 3 | 38 (34.5) | ||
| Schooling after transplantation, n (%) | |||
| Resumed | 28 (25.7) | Follow up, median years after HSCT (range) | 22.8 (11.7-30.3) |
| Completed | 58 (48.7) | ||
| Given up | 23 (25.6) | Acute GvHD (I-IV), n (%) | 39 (35.8) |
| Grade I-II | 35 (89.7) | ||
| Education level, n (%) | Grade III-IV | 4 (10.3) | |
| Compulsory school | 28 (25.7) | ||
| High school | 61 (56) | Chronic GvHD, n (%) | 20 (18.3) |
| University degree or higher | 20 (18.3) | Limited | 13 (65) |
| Extensive | 7 (35) | ||
| Employment status, n (%) | |||
| Unemployed | 19 (17.4) | Comorbidity, n (%) | |
| Employed | 84 (77.1) | Total | 81 (74.3) |
| Inactive* | 6 (5.5) | Metabolic or endocrine | 34 (42.0) |
| Hepatic | 32 (39.5) | ||
| Type of work, n (%) | Cardiac | 27 (33.3) | |
| Full-time employment | 30 (27.6) | Gastrointestinal | 6 (7.4) |
| Part-time employment | 9 (8.3) | Neurologic | 6 (7.4) |
| Self-employed/other | 43 (39.5) | Renal | 5 (6.2) |
| Housewife | 2 (1.8) | Cutaneous | 5 (6.2) |
| Infective | 3 (3.7) | ||
| Marital status, n (%) | Pulmonary | 2 (2.5) | |
| Single | 60 (55) | Solid organ transplant after HSCT | 2 (2.5) |
| Married/Living with partner | 49 (45) | Secondary malignancy | 4 (4.9) |
| Living arrangements, n (%) | Children after HSCT, n (%) | ||
| Living alone | 15 (13.8) | Yes | 17 (15.6%) |
| Living with parents or other relatives | 45 (41.3) | No | 92 (84.4%) |
| Living with spouse/partner | 49 (44.9) | ||
| No. of total healthy births | 23 | ||
Inactive is defined as unemployed and not looking for work.
HRQoL of the transplanted population compared with general population norms
The SF-36 scale scores and the adjusted mean differences between transplanted patients and controls are shown in Table 2. Clinically meaningful differences were observed between population norms and patients for the GH scale (−8.9; 95% CI, −15.0 to 2.7; P = .005). No significant differences were observed for all of the remaining physical and mental health domains. In univariate analysis, patients with comorbidities at the time of the survey had significantly lower scores on the GH scale compared with patients without comorbidities (63.3 vs 84.4, P < .0001). Additional analysis conducted to compare the HRQoL profile of our patients with that of a comparable cohort of nontransplanted thalassemia patients displayed worse outcomes for nontransplanted patients. In particular, clinically meaningful differences were observed for the RP, BP, and RE scales (Figure 1).
Comparisons of SF-36 scale scores between patients transplanted for thalassemia and matched controls from the general population
| SF-36 scales . | Transplanted patients, mean (SD) . | Matched control group, mean (SD) . | Mean difference* (95% CI) . | P value . |
|---|---|---|---|---|
| Physical health | ||||
| Physical functioning | 92.7 (14.1) | 92.0 (15.3) | −2.6 (−7.1; 1.9) | .250 |
| Role physical | 94.5 (10.4) | 88.8 (26.2) | 3.1 (−3.1; 9.2) | .324 |
| Bodily pain | 84.5 (23.6) | 79.1 (24.1) | −0.2 (−7.3; 7.0) | .965 |
| General health | 69.9 (24.1) | 72.2 (17.5) | −8.9 (−15.0; 2.7)† | .005‡ |
| PCS | 53.0 (6.4) | 53.2 (7.4) | −2.1 (−4.1; 0.0) | .05 |
| Mental health | ||||
| Vitality | 69.9 (19.5) | 67.5 (16.5) | −1.9 (−7.3; 3.6) | .499 |
| Social functioning | 82.6 (23.6) | 78.2 (20.2) | 0.7 (−6.2; 7.5) | .851 |
| Role emotional | 92.1 (14.3) | 82.9 (30.6) | 7.0 (−0.5; 14.5) | .068 |
| Mental health | 77.3 (17.5) | 70.3 (16.6) | 4.9 (−0.3; 10.1) | .065 |
| MCS | 54.1 (8.3) | 51.0 (8.5) | 2.0 (−0.6; 4.7) | .127 |
| SF-36 scales . | Transplanted patients, mean (SD) . | Matched control group, mean (SD) . | Mean difference* (95% CI) . | P value . |
|---|---|---|---|---|
| Physical health | ||||
| Physical functioning | 92.7 (14.1) | 92.0 (15.3) | −2.6 (−7.1; 1.9) | .250 |
| Role physical | 94.5 (10.4) | 88.8 (26.2) | 3.1 (−3.1; 9.2) | .324 |
| Bodily pain | 84.5 (23.6) | 79.1 (24.1) | −0.2 (−7.3; 7.0) | .965 |
| General health | 69.9 (24.1) | 72.2 (17.5) | −8.9 (−15.0; 2.7)† | .005‡ |
| PCS | 53.0 (6.4) | 53.2 (7.4) | −2.1 (−4.1; 0.0) | .05 |
| Mental health | ||||
| Vitality | 69.9 (19.5) | 67.5 (16.5) | −1.9 (−7.3; 3.6) | .499 |
| Social functioning | 82.6 (23.6) | 78.2 (20.2) | 0.7 (−6.2; 7.5) | .851 |
| Role emotional | 92.1 (14.3) | 82.9 (30.6) | 7.0 (−0.5; 14.5) | .068 |
| Mental health | 77.3 (17.5) | 70.3 (16.6) | 4.9 (−0.3; 10.1) | .065 |
| MCS | 54.1 (8.3) | 51.0 (8.5) | 2.0 (−0.6; 4.7) | .127 |
Mean differences adjusted for age, gender, education, marital status, and comorbidity.
Exceeds minimally important difference (8 points for SF-36 scales and 2 points for PCS and MCS scales).
Statistically significant after Bonferroni’s correction (adjusted α = 0.05/8 = 0.00625).
Age- and gender-adjusted mean differences of SF-36 scale scores in transplanted patients (n = 109) and a cohort of conventionally treated thalassemia patients (n = 124). The dimensions included physical functioning (PF), role limitations due to physical functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional functioning (RE), and mental health (MH). Scores for all dimensions are expressed on a 0 to 100 scale, where higher scores indicate better health and well-being. Whiskers indicate the standard deviation (±SD) of the SF-36 scale scores. §Clinically meaningful differences between the 2 groups for the RP, BP, and RE scales (score difference of at least 8 points).
Age- and gender-adjusted mean differences of SF-36 scale scores in transplanted patients (n = 109) and a cohort of conventionally treated thalassemia patients (n = 124). The dimensions included physical functioning (PF), role limitations due to physical functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional functioning (RE), and mental health (MH). Scores for all dimensions are expressed on a 0 to 100 scale, where higher scores indicate better health and well-being. Whiskers indicate the standard deviation (±SD) of the SF-36 scale scores. §Clinically meaningful differences between the 2 groups for the RP, BP, and RE scales (score difference of at least 8 points).
Impact of GVHD and age on HRQoL
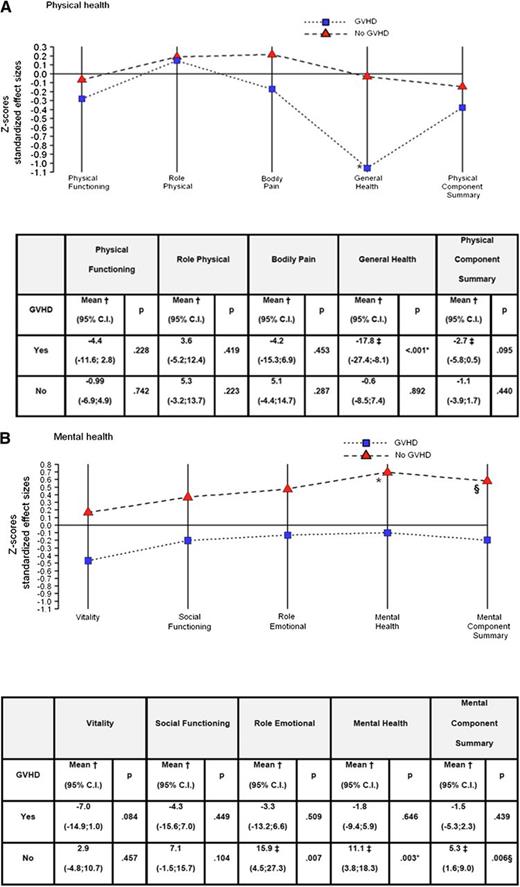
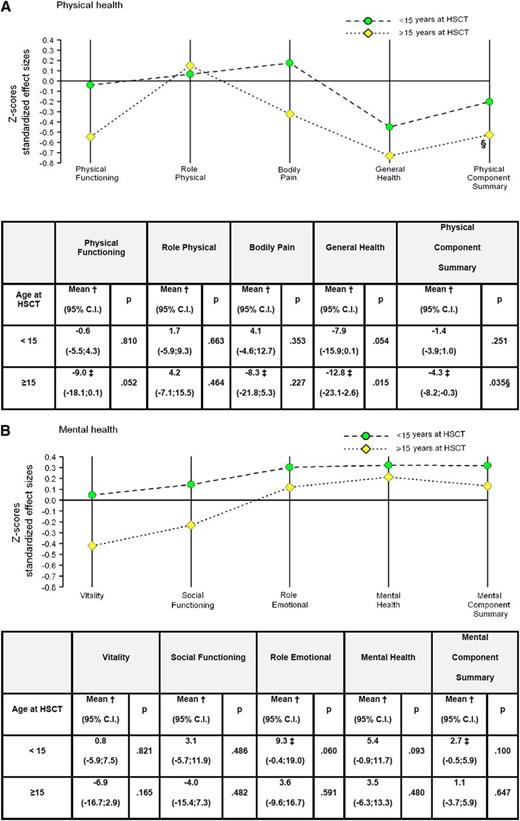
Adjusted mean differences of SF-36 scale scores obtained in patients with (n = 47) or without (n = 62) acute or chronic GVHD and controls are reported in Figure 2. Compared with population norms, patients who developed GVHD after HSCT had significantly worse scores on the GH perception scale (−17.8; 95% CI, −27.4 to −8.1; P < .001). Conversely, patients without GVHD had clinically meaningful scores that were better than those of the control population for the following mental scales: MH (11.1; 95% CI, 3.8-18.3; P = .003), RE (15.9; 95% CI, 4.5-27.3; P = .007), and MCS (5.3; 95% CI, 1.6-9; P = .006). Figure 3 shows the adjusted mean differences for physical and mental domains obtained in patients transplanted before (n = 70) or after (n = 39) the age of 15 years and controls. Worse clinically meaningful scores were observed in the latter group of patients for GH (−12.8; 95% CI, −23.1 to −2.6; P = .015) and PCS (−4.3; 95% CI, −8.2 to −0.3; P = .035). Moreover, univariate analysis showed a significantly higher incidence of comorbidities at the time of the survey in the group of patients with GVHD compared with those without (P = .003).
Adjusted mean differences of the SF-36 scale scores obtained in patients with or without acute or chronic GVHD and controls. (A) Physical health and (B) mental health. A score below line 0 means a worse outcome for HSCT. Note that connecting lines among SF-36 outcomes are plotted for descriptive purposes only. *Statistically significant after Bonferroni’s correction (adjusted α = 0.05/8 = 0.00625). Statistical significance refers to comparisons of SF-36 scores between transplanted patients and matched control subjects. †Mean differences between transplanted patients and matched control subjects adjusted for age, gender, education, marital status, and comorbidity. A negative sign indicates worse outcomes for transplanted patients. ‡Exceeds minimally important difference (ie, 8 points for SF-36 scales and 2 points for PCS and MCS scales). §Statistically significant (α = 0.05).
Adjusted mean differences of the SF-36 scale scores obtained in patients with or without acute or chronic GVHD and controls. (A) Physical health and (B) mental health. A score below line 0 means a worse outcome for HSCT. Note that connecting lines among SF-36 outcomes are plotted for descriptive purposes only. *Statistically significant after Bonferroni’s correction (adjusted α = 0.05/8 = 0.00625). Statistical significance refers to comparisons of SF-36 scores between transplanted patients and matched control subjects. †Mean differences between transplanted patients and matched control subjects adjusted for age, gender, education, marital status, and comorbidity. A negative sign indicates worse outcomes for transplanted patients. ‡Exceeds minimally important difference (ie, 8 points for SF-36 scales and 2 points for PCS and MCS scales). §Statistically significant (α = 0.05).
Adjusted mean differences for physical and health domains obtained in patients, transplanted before or after the age of 15 years, and controls. (A) Physical health and (B) mental health. A score below line 0 means worse outcomes for transplanted patients. Note that connecting lines among SF-36 outcomes are plotted for descriptive purposes only. †Mean differences between transplanted patients and matched control subjects adjusted for age, gender, education, marital status, and comorbidity. A negative sign indicates worse outcomes for transplanted patients. ‡Exceeds minimally important difference (ie, 8 points for SF-36 scales and 2 points for PCS and MCS scales). §Statistically significant (α = 0.05).
Adjusted mean differences for physical and health domains obtained in patients, transplanted before or after the age of 15 years, and controls. (A) Physical health and (B) mental health. A score below line 0 means worse outcomes for transplanted patients. Note that connecting lines among SF-36 outcomes are plotted for descriptive purposes only. †Mean differences between transplanted patients and matched control subjects adjusted for age, gender, education, marital status, and comorbidity. A negative sign indicates worse outcomes for transplanted patients. ‡Exceeds minimally important difference (ie, 8 points for SF-36 scales and 2 points for PCS and MCS scales). §Statistically significant (α = 0.05).
Factors associated with HRQoL outcomes
Total scores of the FACT-BMT in our cohort of transplanted ex-thalassemia patients confirmed the association of GVHD with worse HRQoL (P = .006). Lower FACT-BMT scores were also registered for patients with comorbidities (P = .031) or living alone (P = .0263) (Table 3).
HRQoL outcomes (FACT-BMT total scores) by key sociodemographic and clinical data
| Variable . | Values . | No . | Yes . | Total . | P value . |
|---|---|---|---|---|---|
| Male | Mean (SD) | 117.43 (17.98) | 123.95 (17.11) | 121.32 (17.68) | .0657 |
| Median | 124.44 | 124.61 | 124.61 | ||
| Range | 71.83-145.00 | 74.08-148.00 | 71.83-148.00 | ||
| n | 44 | 65 | 109 | ||
| Living alone | Mean (SD) | 122.76 (17.14) | 112.28 (18.93) | 121.32 (17.68) | .0263 |
| Median | 125.47 | 115.67 | 124.61 | ||
| Range | 71.83-148.00 | 77.50-146.89 | 71.83-148.00 | ||
| n | 94 | 15 | 109 | ||
| Secondary school or higher | Mean (SD) | 113.33 (22.92) | 124.08 (14.65) | 121.32 (17.68) | .0501 |
| Median | 125.78 | 117.28 | 124.61 | ||
| Range | 85.25-148.00 | 71.83-147.00 | 71.83-148.00 | ||
| n | 81 | 28 | 109 | ||
| GVHD | Mean (SD) | 125.00 (16.38) | 116.47 (18.33) | 121.32 (17.68) | .0067 |
| Median | 127.03 | 116.78 | 124.61 | ||
| Range | 74.08-148.00 | 71.83-145.00 | 71.83-148.00 | ||
| n | 62 | 47 | 109 | ||
| Comorbidity at survey | Mean (SD) | 127.26 (13.19) | 118.74 (18.81) | 121.32 (17.68) | .0318 |
| Median | 129.39 | 123.81 | 124.61 | ||
| Range | 91.44-147.00 | 71.83-148.00 | 71.83-148.00 | ||
| n | 33 | 76 | 109 |
| Variable . | Values . | No . | Yes . | Total . | P value . |
|---|---|---|---|---|---|
| Male | Mean (SD) | 117.43 (17.98) | 123.95 (17.11) | 121.32 (17.68) | .0657 |
| Median | 124.44 | 124.61 | 124.61 | ||
| Range | 71.83-145.00 | 74.08-148.00 | 71.83-148.00 | ||
| n | 44 | 65 | 109 | ||
| Living alone | Mean (SD) | 122.76 (17.14) | 112.28 (18.93) | 121.32 (17.68) | .0263 |
| Median | 125.47 | 115.67 | 124.61 | ||
| Range | 71.83-148.00 | 77.50-146.89 | 71.83-148.00 | ||
| n | 94 | 15 | 109 | ||
| Secondary school or higher | Mean (SD) | 113.33 (22.92) | 124.08 (14.65) | 121.32 (17.68) | .0501 |
| Median | 125.78 | 117.28 | 124.61 | ||
| Range | 85.25-148.00 | 71.83-147.00 | 71.83-148.00 | ||
| n | 81 | 28 | 109 | ||
| GVHD | Mean (SD) | 125.00 (16.38) | 116.47 (18.33) | 121.32 (17.68) | .0067 |
| Median | 127.03 | 116.78 | 124.61 | ||
| Range | 74.08-148.00 | 71.83-145.00 | 71.83-148.00 | ||
| n | 62 | 47 | 109 | ||
| Comorbidity at survey | Mean (SD) | 127.26 (13.19) | 118.74 (18.81) | 121.32 (17.68) | .0318 |
| Median | 129.39 | 123.81 | 124.61 | ||
| Range | 91.44-147.00 | 71.83-148.00 | 71.83-148.00 | ||
| n | 33 | 76 | 109 |
Discussion
Overall, our study shows that the long-term HRQoL profile of patients transplanted for β-thalassemia is broadly similar to that of their peers from the general population. In addition, when compared with conventionally treated patients, transplanted patients had a better HRQoL profile. Patients recover well and seem to regain good levels of both mental and physical performance in the long term. However, those patients in our study who had acute or chronic GVHD reported significant limitations of physical performance (GH scale of the SF-36) (Figure 2). In addition, GVHD had a negative impact on the incidence of comorbidities. Conversely, the group of patients without GVHD, independent of age at HSCT, reported scores for mental health that were even higher than those of their respective peers in the general population. This latter finding could be a consequence of the strong motivational drive of patients with a history of chronic disease who consider HSCT as a possibility of a new beginning. A similar explanation, in which patients attribute a new meaning to life, has been suggested for the better QoL reported by long-term pediatric cancer survivors compared with the general population.37
In our study, acute or chronic GvHD was also associated with lower scores on several scales of the FACT-BMT questionnaire (Table 3), thus emphasizing the impairing role of GVHD on QoL. Notably, all 4 patients who developed a secondary malignancy had chronic GVHD. All of these findings indicate the need to further reduce the incidence of GVHD and thus to limit its negative effects on physical functioning in the long term. An important role has been suggested for antithymocyte globulin (ATG) in reducing the incidence and severity of acute and chronic GVHD with a positive rebound on all aspects of QoL.38
Our results also seem to indicate that patients who undergo HSCT at a younger age (<15 years) are more likely to achieve better long-term HRQoL outcomes (Figure 3). Indeed, these patients basically show a physical and mental health profile that is very similar to that of their peers in the general population. A possible explanation is that younger patients are less exposed to the risk of organ damage caused by iron overload and have a lower risk of developing GVHD.39 Notably, the 6 female patients who gave birth to a total of 7 healthy children had all undergone HSCT before the age of 15 years. Overall, these data suggest that, whenever possible, HSCT should be performed in pediatric years.
A secondary end point of our study was to evaluate the impact of clinical and sociodemographic factors on HRQoL outcomes. Patients who reported the presence of a comorbidity at the time of the survey and those living alone had worse FACT-BMT total scores (Table 3). Most patients (74.3%) had at least 1 disorder at the time of the survey. Within this context, it is important to mention that 35% of our patients belonged to the Class 3 high-risk category, which is characterized by irregular pretransplantation iron chelation, hepatomegaly, and the presence of portal fibrosis.24 A high incidence was registered for HCV hepatitis (Table 1). However, the majority of our patients had undergone transplant before blood components for transfusion purposes could be tested for the presence of HCV. Screening tests for HCV became available in 1990, and since then they have drastically reduced the incidence of infections in polytransfused thalassemia patients.
Despite the high incidence of comorbidities, our cohort of ex-thalassemia patients led a normal life, reporting daily activities and living patterns similar to those of the general population. The birth rate in our cohort was similar to previously published data from long-term HSCT surviving thalassemia patients22 and was higher than that registered in 2011 for the Sardinian population.40 Most of our patients had completed their studies after HSCT, achieving education levels in similar proportion to data provided for the general population.41 Notwithstanding the current difficult economic scenery, 77% of our patients held a job position. Interestingly, this percentage is higher than the 59.9% employment rate reported by the Italian National Institute of Statistics for individuals of the Sardinian population aged 20 to 45 years.42 When considering marital status, we found that the condition of “single” was more frequent among transplanted patients than in the general population (55% vs 30%).43 Only 13.8% of our patients lived alone, resulting in significantly worse HRQoL outcomes (Table 3). However, the apparent high rate of transplanted patients living with at least 1 parent or relative (41.3%) was no different from the rate registered in a comparable population (43.3%) in Italy.44
Despite these interesting results, the present study has some limitations. Because of its cross-sectional design, we were unable to analyze HRQoL compared with baseline values. In addition, all patients came from the island of Sardinia, and we did not recruit patients from other geographical areas.
In conclusion, although our findings provide clear evidence of good HRQoL and return to normal life style in long-term ex-thalassemia patients, the choice of undergoing HSCT remains difficult. Over the past few years, the availability of oral iron chelators and increasingly safe and efficient transfusion therapy has radically improved the life expectancy of thalassemia patients. On the other hand, HSCT offers patients the possibility of a definitive cure with a relatively low risk of transplantation-related mortality. The availability of novel data on HRQoL in the long term should provide both physicians and patients with a better comprehension of the advantages and potential risks of HSCT and assist them in the treatment decision-making process.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Antonello Antonelli of the Public Health Department of the Sardinian Regional Government for his precious collaboration; Dr Giovanni Spanu and Dr Samantha Pinna (Bone Marrow Transplant Center, R. Binaghi Hospital, Cagliari, Italy) for data collection; and Anna Maria Koopmans (Bone Marrow Transplant Center and Regional Transplant Center, R. Binaghi Hospital, Cagliari, Italy) for her professional assistance in writing the manuscript.
Authorship
Contribution: G.L.N. and G.C. designed and coordinated the study, interpreted data and wrote the first draft; F.E. coordinated analyses and interpretation of data and critically reviewed the final draft; A.V., E.P., M.S., and R.L. recruited patients and administered and analyzed survey instruments; C.D. and M.M. recruited conventionally treated thalassemia patients and administered and analyzed survey instruments; C.C. contributed to data analyses and interpretation; and G.L. designed and coordinated the study and critically reviewed the final draft.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Giorgio La Nasa, Bone Marrow Transplant Center, R. Binaghi Hospital, Via Is Guadazzonis 3, 09126 Cagliari, Italy; e-mail: lanasa@tiscali.it.
References
Author notes
G.L.N. and G.C. contributed equally to this study.