Key Points
Mature, but not immature, dendritic cells are sensitive to glucocorticoid-induced apoptosis.
Mature, but not immature, dendritic cells express proapoptotic glucocorticoid receptor translational isoforms.
Abstract
Although glucocorticoids are a profoundly important class of anti-inflammatory and immunosuppressive agents, their actions in dendritic cells (DCs) are not well understood. We found that dexamethasone, a potent glucocorticoid, selectively induced apoptosis in mature, but not in immature, DCs in healthy mice, in mice with experimental airway inflammation, and in vitro in bone marrow–derived DCs. Distinct glucocorticoid receptor (GR) translational isoforms expressed in immature and mature DCs probably contribute to the DC maturational stage-specific glucocorticoid sensitivity. The GR-D isoforms were the predominant isoforms in immature DCs, whereas the proapoptotic GR-A isoform was the main isoform in mature DCs. Ectopic expression of the GR-A isoform in immature DCs increased glucocorticoid sensitivity and RU486, a selective GR antagonist, inhibited the glucocorticoid sensitivity of mature DCs. Furthermore, the distinct expression pattern of GR isoforms in immature and mature murine DCs was also observed in human monocyte–derived DCs. These studies suggest that glucocorticoids may spare immature DCs and suppress mature DCs and inflammation via differential expression of GR translational isoforms.
Introduction
Dendritic cells (DCs) are sentinel cells of adaptive immune responses.1-4 Based on the expression level of major histocompatibility complex (MHC) II and costimulatory molecules, DCs have been categorized into immature and mature DCs. During inflammation, immature DCs react to pathogen-derived molecules such as lipopolysaccharide (LPS) and undergo maturation. DCs can also be categorized into proinflammatory DCs and tolerogenic DCs based on their influence on the immune response. Mature DCs are the most potent antigen-presenting cells that initiate adaptive immune responses. On the other hand, immature DCs and DCs matured by harmless environmental stimuli and certain pathogens contribute to tolerance.2,3,5 Because DC subsets are numerous and their functional categorization is complex, and because their numbers are low, our understanding of the responsiveness of DC subsets to anti-inflammatory drugs is limited.
Glucocorticoids are an important class of anti-inflammatory and immunosuppressive drugs widely prescribed for numerous inflammatory conditions.6 However, long-term glucocorticoid usage can cause serious side effects such as hypertension and osteoporosis and can compromise the immune system. Therefore, there is a need to improve the efficacy/risk ratio of glucocorticoids. The anti-inflammatory benefits of glucocorticoids have been attributed in part to their actions in various immune cells. It has been reported that DC maturation is suppressed by glucocorticoids.7,8 Addition of glucocorticoids during DC activation results in reduced expression of surface MHC II and costimulatory molecules, suppressed proinflammatory cytokines, and increased interleukin (IL)–10 production.8-14 Antigen processing and presentation by DCs are almost completely inhibited when antigen pulsing is performed in the presence of glucocorticoids.11,12,15 Consequently, glucocorticoids impair T-cell stimulatory capacity of DCs.13,14,16,17 In addition, glucocorticoids may reduce the number of DCs via inhibiting DC migration and increasing DC apoptosis,7,9,10,12,15,18-25 although some other reports suggest that glucocorticoids do not induce DCs apoptosis.13,16,26,27 It is not known whether different DC subsets have differential sensitivity to glucocorticoid-induced apoptosis.
Both the beneficial and deleterious effects of glucocorticoids are mediated by the glucocorticoid receptor (GR). Our previous work showed that 1 GR gene encodes multiple GR isoforms including GRα and β generated by alternative splicing and GRα-A, B, C1, C2, C3, D1, D2, and D3 isoforms generated via alternative translation initiation mechanisms.28 Although various GR isoforms have distinct tissue distribution patterns, the level of GRα is significantly higher than that of GRβ29 and GRβ does not appear to play a role in glucocorticoid actions in DCs.30 On activation by glucocorticoids, GR mainly acts at the transcriptional level to suppress the expression of proinflammatory genes and to induce anti-inflammatory genes.6 Different GR isoforms have different sets of gene targets.28,31 In addition, all GR translational isoforms, except the GR-D isoforms, are proapoptotic in U-2 OS cells, an osteoblast cell line, by inducing proapoptotic genes and repressing antiapoptotic genes.31,32 Although it has been demonstrated that DCs contain GR,9,10,25 the identity of GR isoforms in DCs has not been determined, and whether various GR isoforms specifically regulate DCs functions is not known.
We report here that mature, but not immature, DCs are sensitive to glucocorticoid-induced apoptosis, and that DCs undergo a switch of GR isoforms during maturation. The killing of mature DCs by dexamethasone (DEX), a potent GR agonist, can be inhibited by RU486, a GR-selective antagonist, and ectopic expression of proapoptotic GR isoforms in immature DCs can induce glucocorticoid sensitivity, suggesting that selective expression of GR translational isoforms in immature and mature DCs probably underlies DC maturational stage-specific sensitivity to glucocorticoids. We also found that DEX inhibits antigen uptake in immature DCs and blocks cytokine production in mature DCs. Thus, glucocorticoids regulate DC functions in a DC maturational stage-specific manner via selective GR isoforms. These studies, together with studies in other cell types, may provide a basis for developing GR isoform-specific compounds with improved benefit-risk ratios.
Methods
Reagents and animals
DEX was from Steraloids. Female Balb/c mice, 6 to 8 weeks old, were from Taconic. Animal usage was approved by the Institutional Animal Care and Use Committee at Northwestern University, no. 2010-1121. Antibody and cytokine sources are listed in supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Murine asthma model
Female Balb/c mice 6 to 8 weeks old were sensitized to OVA according to a published protocol33 with 2 intraperitoneal injections of 10 μg ovalbumin (OVA; EndoGrade, BioVendor) and alum (3 mg) on days 0 and 14. On days 21, 22, and 23, mice were challenged intratracheally with OVA (500 μg in 50 μL sterile PBS). Control mice received alum sensitization and PBS challenge. Animals were treated with vehicle or DEX (5 mg/kg, intraperitoneally) 5 days after the last challenge. Bronchoalveolar lavages (BALs), mediastinal lymph nodes, lungs, and spleens were obtained 24 hours after DEX treatment. Hematoxylin and eosin-stained lung sections were imaged on an Olympus IX71 microscope using a 10× objective at room temperature. Images were captured using an Optronics Microfire camera. Image acquisition and layout softwares were Optronics PictureFrame 2.3 and Abobe Photoshop 8.0, respectively.
Immunofluorescent histochemistry
For staining of the active form of caspase 3, prepared sections (supplemental Methods), were then incubated with rabbit anti–caspase-3 (1:4000), followed by biotinylated goat anti–rabbit antibodies (1:200), streptavidin-HRP (1:200), and coumarin tyramide (1:100). For staining of CD11c and MHC II, slides were washed with TNT buffer and incubated with 10% normal goat serum, followed by Armenian hamster anti–mouse CD11c (1:300) and rat anti–mouse MHC II antibodies (1:600). After washing, slides were incubated with DyLight488 conjugated goat anti–Armenian hamster antibodies (1:300) and Texas red conjugated goat anti–rat antibodies (1:600), mounted with Fluoromount-G (SouthernBiotech), and imaged on a Nikon Eclipse E800 fluorescent microscope using a 40× objective at room temperature. Slides processed without primary antibodies were used as controls. Images were captured using a Photometrics CoolSNAP HQ camera. Image acquisition and layout softwares were Photometrics MetaMorph 6.1 and Abobe Photoshop 8.0, respectively.
DC culture
Bone marrow–derived DCs (BMDCs) were cultured as previously described.34 Briefly, bone marrow was harvested from femurs and tibiae of Balb/c mice (female, 6-8 weeks old) and cultured in complete RPMI medium (Invitrogen) containing 10% US defined fetal bovine serum (FBS; HyClone), 2mM glutamine, 50 U/mL penicillin, and 50 μg/mL streptomycin supplemented with mouse GM-CSF (20 ng/mL) in a 5% CO2 atmosphere at 37°C. Medium was replenished on days 3, 5, and 8 of culture. After 8 days in culture, approximately 90% of the cells were CD11c+ DCs. DC maturation was stimulated using LPS (0.01 to 10 ng/mL) or LTA (4 μg/mL) for 24 to 48 hours. For apoptosis assays, live immature (DAPI−CD11c+CD86−/lowMHC II−/low) and mature (DAPI−CD11c+CD86high [hi] MHC IIhi) DCs were sorted on a MoFlo cell sorter to greater than 97% purity. Sorted cells were treated with DEX (100nM) ± RU486 (100nM) in growth media supplemented with 5% charcoal-dextran stripped FBS for 24 hours before apoptosis assays.
To generate human monocyte–derived DCs according to established protocol, monocytes were purified from peripheral blood mononuclear cells (American Red Cross) using the Human Monocyte Enrichment kits (negative selection, StemCell Technologies). Monocytes were cultured in complete RPMI medium supplemented with 100 ng/mL human GM-CSF and IL-4. Medium was replenished every other day. After 8 days in culture, characteristic DC morphology was observed and CD14−CD1a+ cells reached approximately 90%. For Western blot analyses, cells were stimulated with vehicle or LPS (1 ng/mL, 24 hours). For apoptosis assays, control or LPS treated cells were further treated with vehicle or DEX (100nM, 48 hours) in growth media supplemented with 5% charcoal-dextran stripped FBS.
Immunocytochemistry
BMDCs were cultured in chamber slides in growth media supplemented with 5% charcoal dextran-stripped FBS and treated with vehicle or LPS (1 ng/mL) ± DEX (10nM) for 24 hours. Cells were fixed with 4% paraformaldehyde and endogenous HRP was quenched using 3% H2O2. Blocking was performed using 5% normal goat serum in PBS containing 0.05% triton x-100. Slides were then incubated with anti-GR #57 (1:100) in blocking solution overnight at 4°C. After washing, slides were incubated with polymer-HRP anti–rabbit (EnVision plus system-HRP, DAKO) for 30 minutes, washed, developed using DAB (DAKO), and imaged on an Olympus IX71 microscope using a 100× objective at room temperature. Slides processed without primary antibodies were used as controls. Images were captured using an Optronics Microfire camera. Image acquisition and layout softwares were Optronics PictureFrame 2.3 and Abobe Photoshop 8.0, respectively.
Transfection of BMDCs
BMDCs cultured with GM-CSF for 7 days were transfected with pTRE-hGR-A28 and pmax-GFP using the Amaxa Nucleofector system (Lonza) according to the manufacturer's protocol. Transfection efficiency was greater than 50%. After transfection, cells were cultured overnight and sorted on a MoFlo cell sorter. Sorted GFP+ cells were treated with vehicle or DEX (100nM) in growth media supplemented with 5% charcoal-dextran stripped FBS for 24 hours before apoptosis assays.
Flow cytometry
Surface staining of single-cell suspensions of cultured BMDCs was performed at 4°C for 30 minutes. Rat and hamster normal serum and rat anti–mouse CD16/32 were used to block background staining. Annexin V, DAPI, and propidium iodide (PI) labeling was processed using the annexin V–FITC apoptosis detection kit (Biovision) according to the manufacturer's instructions. After washing, cells were analyzed on an LSR II flow cytometer (Becton Dickinson). Data analysis was conducted using FACSDiva software (Becton Dickinson), and FCSexpress (De Novo Software).
Cytometric bead array
Mouse inflammation cytometric bead array (CBA) kit (BD Biosciences) was used to measure cytokines secreted by BMDCs treated with vehicle or LPS (1 ng/mL) ± DEX (10nM) for 24 hours. Supernatants were cleared of debris and subjected to CBA analysis to measure the levels of IL-6 and tumor necrosis factor (TNF)–α according to the manufacturer's protocol.
Mixed leukocyte reaction
Control or LPS (1 ng/mL, 24 hours)–activated BMDCs were treated with vehicle or DEX (10nM) for 24 hours and cocultured according to the established protocol35 with CD4+ T cells isolated using Miltenyi kits and labeled with carboxyfluorescein diacetate succinimidyl ester (CFSE, Invitrogen) according to the manufacturer's instruction. CFSE signal was detected after 5 days of coculture on an LSRII flow cytometer.
Uptake assay
Control or LPS (1 ng/mL, 24 hours)–activated BMDCs were treated with vehicle or DEX (10nM) for 24 hours and incubated with 1 mg/mL FITC-dextran (average molecular weight 2000 Kd, Sigma-Aldrich) in growth media at 4°C or 37°C for 10 to 40 minutes. After washing 3 times with ice-cold PBS, cells were labeled on ice with PEcy7-CD11c. Intracellular FITC signals of CD11c+ cells were measured on an LSRII flow cytometer. The amount of FITC-dextran uptake was calculated as the change in mean fluorescence intensity between samples incubated at 37°C and 4°C.
Western blot analysis
Procedures for preparing cell lysates for Western blot analysis were previously described.28 The titers for primary antibodies were: anti-GR #57 antibodies (1:400) and anti-actin (1:600 000). HRP-conjugated anti–rabbit antibodies were used at 1:10 000 dilution for 30 minutes. After washing, membranes were probed with ECL reagent (GE Amersham) and exposed to ECL film (GE Amersham).
Realtime RT-PCR and PCR Arrays
RNA samples were extracted from BMDCs treated with vehicle or LPS (1 ng/mL, 0-24 hours) ± DEX (100nM, 6 hours) using the Absolutely RNA RT-PCR Miniprep Kit (Stratagene) and treated with DNase according to the manufacturer's protocol. The level of specific mRNA in each sample was measured using the 1-step RT-PCR procedure on a Prism 7500HT thermocycler (Applied Biosystems) as previously described.28 Each experiment was performed in duplicate with at least 3 biologic replicates. Quantification was achieved using the Sequence Detection Software 2.0 Absolute Level subroutine (Applied Biosystems). Primer information is in supplemental Methods. Mouse Apoptosis PCR Arrays were performed according to the manufacturer's protocol starting with 0.5 μg of RNA for each plate. Results (n = 3) were normalized using B2m gene and analyzed using the manufacturer's Web software.
Statistical analysis
For comparison of 2 groups, Student t test was performed. For comparison of 3 or more treatment groups, 1-way ANOVA was performed followed by the Tukey posthoc comparison using Prism 4 software (GraphPad). A P value < .05 was considered significant.
Results
Selective activation of caspase 3 in mature, but not in immature, DCs in murine spleen by DEX
To clarify the conflicting data in the literature regarding glucocorticoid sensitivity of DCs, we determined whether immature and mature DCs have different sensitivity to glucocorticoid-induced apoptosis. Triple immunostaining was performed on mouse splenic DCs using DCs markers CD11c and MHC II and an apoptosis marker, caspase 3 (Figure 1). Immature DCs were defined as CD11c+MHC II−/low whereas mature DCs were defined as CD11c+MHC IIhigh (hi). These definitions and the inclusion of cells from both T-cell areas and interfollicular areas of the marginal zone encompass various subsets of DCs. In spleens of naive mice, the majority of DCs are CD11c+CD8−CD205−CD11b+ (70%) and CD11c+CD8hiCD205+CD11b− (23%).4 In contrast, migratory (CD11c+CD8−CD205+CD11b+) and plasmacytoid (CD11c intermediate B220+Ly6C/6G+) DCs constitute less than 4%, and 2% to 3% of DCs in murine spleens, respectively. In addition to staining all DCs in spleen, CD11c may also label a small number of activated T cells and natural killer cells, which can be distinguished from DCs by their morphology. Activated caspase 3 was used as a marker for apoptosis. After treatment with a potent glucocorticoid, DEX (5 mg/kg, intraperitoneally, 24 hours), a significantly higher percentage of mature DCs (35.2 ± 10.8, mean ± SD) than immature DCs (4.3 ± 1.3, mean ± SD) had caspase 3 activation (Figure 1). Control sections from vehicle treated animals had little caspase 3 activation (Figure 1). These observations indicate that mature, but not immature, DCs are susceptible to DEX-killing in vivo in spleens of naive mice.
Distinct glucocorticoid sensitivities of immature and mature DCs in murine spleen. (A) Triple immunostaining shows caspase 3 activation in DCs on spleen sections in control (CON) and DEX (5 mg/kg, intraperitoneally, 24 hours) treated animals. Immature DCs (white arrows) in mouse spleen sections were CD11c+MHC II−/low whereas mature DCs (red arrows) were CD11c+MHC IIhigh. CD11c, MHC II, and activated caspase 3 signals were indicated in green, red, and blue, respectively. Sections from control animals showed few cells with activated caspase 3 staining. Bright field images of hematoxylin and eosin stained sections indicate the cell numbers. Scale bar, 20 μm. (B) Percentages (± SD) of caspase 3+ cells were compared between CON and DEX. Approximately 150 to 600 cells per animal (n = 6 per group) were counted across 3 to 12 sections (*significantly greater than CON; P < .0001, Student t test).
Distinct glucocorticoid sensitivities of immature and mature DCs in murine spleen. (A) Triple immunostaining shows caspase 3 activation in DCs on spleen sections in control (CON) and DEX (5 mg/kg, intraperitoneally, 24 hours) treated animals. Immature DCs (white arrows) in mouse spleen sections were CD11c+MHC II−/low whereas mature DCs (red arrows) were CD11c+MHC IIhigh. CD11c, MHC II, and activated caspase 3 signals were indicated in green, red, and blue, respectively. Sections from control animals showed few cells with activated caspase 3 staining. Bright field images of hematoxylin and eosin stained sections indicate the cell numbers. Scale bar, 20 μm. (B) Percentages (± SD) of caspase 3+ cells were compared between CON and DEX. Approximately 150 to 600 cells per animal (n = 6 per group) were counted across 3 to 12 sections (*significantly greater than CON; P < .0001, Student t test).
Selective activation of caspase 3 in mature, but not in immature, DCs in draining lymph nodes by DEX in a murine asthma model
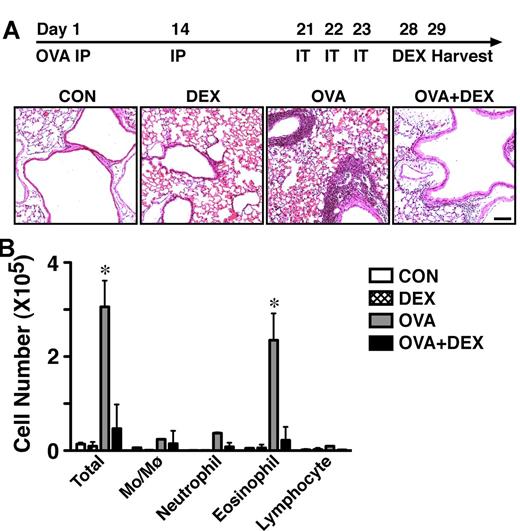
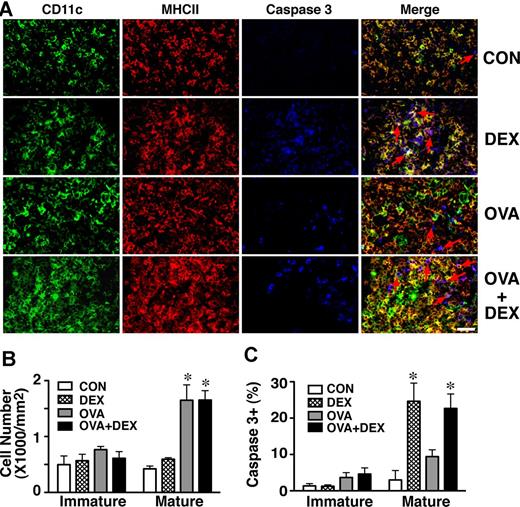
DCs in draining lymph nodes are composed of resident DCs and migratory DCs.4 Inflammation triggers not only maturation of resident DCs and influx of mature DCs, but also recruitment of DCs converted from monocytes.3 We used the OVA murine asthma model (Figure 2) to examine the glucocorticoid sensitivity of DCs during inflammation. OVA-induced leukocyte infiltration, epithelial hyperplasia, and eosinophil recruitment are shown in Figure 2A and B and the anti-inflammatory effects of DEX (5 mg/kg, intraperitoneally, 24 hours) were evident. Previous reports indicate that glucocorticoids inhibit DC maturation and antigen presentation in the presence of inflammatory stimuli. Therefore, to examine the glucocorticoid sensitivity of both immature and mature DCs, we completed sensitization and challenges with OVA to allow DCs to undergo maturation before DEX treatments (Figure 2A). Triple immunostaining for CD11c, MHC II, and caspase 3 was performed on mediastinal lymph node sections from control, OVA, DEX, and OVA+DEX treated groups (Figure 3). Experimental asthma caused an approximately 2-fold increase in the number of mature DCs in mediastinal lymph nodes, although the number of immature DCs did not change significantly after the asthma regimen (Figure 3B). Moreover, DEX significantly increased the caspase 3 signal in mature, but not in immature, DCs (Figure 3A-C). The percentages (mean ± SD) of apoptotic cells were 1.4 ± 0.6, 1.3 ± 0.4, 3.7 ± 1.3, and 4.6 ± 1.7 for immature DCs and 3.0 ± 2.6, 24.7 ± 5.0, 9.4 ± 1.9, and 22.7 ± 4.0 for mature DCs treated with vehicle, DEX, OVA, and OVA+DEX, respectively. These findings obtained from an inflammatory model system confirm the observations made in resting spleens (as described in the previous section). In both scenarios mature, but not immature, DCs were sensitive to DEX-induced caspase 3 activation in vivo.
OVA experimental asthma model. (A) Two IP sensitizing doses of OVA and 3 IT challenges were given on indicated days. Hematoxylin and eosin staining of lung sections indicates the infiltration of leukocytes and airway thickening of OVA-treated animals. DEX (5 mg/kg, intraperitoneally, 24 hours) reduced the number of leukocytes in lungs (n = 6). Scale bar, 1 mm. (B) Differential cell counts (averages ± SD) of the bronchoalveolar lavage indicated that OVA-treatment elevated the eosinophil number, a process that was blocked by DEX (n = 6; *significantly greater than CON, P < .01; 1-way ANOVA followed by Tukey posthoc test).
OVA experimental asthma model. (A) Two IP sensitizing doses of OVA and 3 IT challenges were given on indicated days. Hematoxylin and eosin staining of lung sections indicates the infiltration of leukocytes and airway thickening of OVA-treated animals. DEX (5 mg/kg, intraperitoneally, 24 hours) reduced the number of leukocytes in lungs (n = 6). Scale bar, 1 mm. (B) Differential cell counts (averages ± SD) of the bronchoalveolar lavage indicated that OVA-treatment elevated the eosinophil number, a process that was blocked by DEX (n = 6; *significantly greater than CON, P < .01; 1-way ANOVA followed by Tukey posthoc test).
Mature DCs in murine lymph nodes are more susceptible to glucocorticoid killing than immature DCs during experimental asthma. (A) Triple immunostaining of CD11c (green), MHC II (red), and caspase 3 (blue) was performed on mediastinal lymph node sections as described in “Methods” and in Figure 1. Merged images contain staining for all 3 antigens and show that the majority of the caspase 3+ cells (red arrows) are mature DCs. Scale bar, 20 μm. (B) OVA treatment increased the number of DCs (± SD) in mediastinal lymph nodes. Approximately 150 (CON and DEX groups) to 900 (OVA and OVA+DEX) cells per animal (n = 6 per group) were counted across 3 to 12 sections. (C) DEX induced caspase 3 activation more efficiently in mature DCs than in immature DCs (*significantly greater than CON, P < .01; 1-way ANOVA followed by Tukey posthoc test).
Mature DCs in murine lymph nodes are more susceptible to glucocorticoid killing than immature DCs during experimental asthma. (A) Triple immunostaining of CD11c (green), MHC II (red), and caspase 3 (blue) was performed on mediastinal lymph node sections as described in “Methods” and in Figure 1. Merged images contain staining for all 3 antigens and show that the majority of the caspase 3+ cells (red arrows) are mature DCs. Scale bar, 20 μm. (B) OVA treatment increased the number of DCs (± SD) in mediastinal lymph nodes. Approximately 150 (CON and DEX groups) to 900 (OVA and OVA+DEX) cells per animal (n = 6 per group) were counted across 3 to 12 sections. (C) DEX induced caspase 3 activation more efficiently in mature DCs than in immature DCs (*significantly greater than CON, P < .01; 1-way ANOVA followed by Tukey posthoc test).
Distinct glucocorticoid responses of immature and mature BMDCs
To determine the role GR isoforms in distinct sensitivity of immature and mature DCs to glucocorticoid-induced apoptosis, we face several obstacles: the scarcity of DCs, the lack of GR translational isoform-specific antibodies because of overlapping sequences of GR isoforms,28 and the requirement for large amounts of DCs (approximately 2 million cells) for successful Western blot detection of GR isoforms. To overcome these obstacles, we used murine BMDCs that provide a reliable source of large numbers of DCs with cell-surface markers similar to those of DCs observed during inflammation.34 BMDCs can reach greater than 90% purity (CD11c+) after 7 days in culture containing GM-CSF. The majority of BMDCs are immature, based on their surface expression of MHC II and CD86 (Figure 4A), cytokine production (Figure 4B), and T-cell activation capability (Figure 4C), before exposure to inflammatory stimuli. LPS (1 ng/mL, 24 hours) significantly increased the expression of MHC II and CD86, the production of TNF-α and IL-6, and T-cell activation. DEX (10nM, 24 hours) suppressed the LPS-induced expression of MHC II and CD86, cytokine production as well as T-cell activation. Figure 4D shows that BMDCs had “probe-like” processes, a signature feature of DC morphology. We performed immunocytochemistry on BMDCs to identify the expression and cellular location of GR (Figure 4D). Both control and LPS-treated BMDCs had prominent GR staining. In the absence of glucocorticoids, immature DCs had GR staining mostly in the nucleus and the perinuclear region, whereas mature BMDCs had GR staining predominantly in the cytoplasm. In the presence of DEX (10nM), both immature and mature BMDCs had GR staining predominantly in the nucleus. We previously reported that the GR-D isoforms are localized in the nucleus whereas the GR-A, B, and C isoforms are in the cytoplasm in the absence of cognate ligands.28 All cytoplasmic GR isoforms translocate into the nucleus in the presence of glucocorticoids. The nuclear localization of the GR-D isoforms in the absence of glucocorticoids suggests that the GR-D isoforms may have glucocorticoid-independent functions in the nucleus. Together, these observations indicate that BMDCs express GR and the GR isoforms in immature and mature BMDCs may be different.
Distinct glucocorticoid responsiveness of BMDCs. (A) Flow cytometric assessment of expression levels of CD86 and MHC II on BMDCs from control (CON), DEX (10nM, 24 hours), LPS (1 ng/mL, 24 hours), and LPS+DEX treated cultures shows that LPS induced both CD86 and MHC II, which was blocked by DEX. Experiments were repeated at least 4 times. (B) LPS (1 ng/mL, 24 hours) significantly induced TNF-α and IL-6 production by BMDCs. DEX (10nM, 24 hours) efficiently blocked the LPS-induced cytokine production. Averages (± SD) from 4 experiments are shown (*significantly greater than other treatment groups, P < .05; 1-way ANOVA followed by Tukey posthoc test). (C) T cell proliferation (CFSE) in CD4+ T cells and LPS-activated BMDC coculture was repressed when BMDCs were pretreated with DEX (10nM, 24 hours). Experiments were repeated at least 4 times. (D) Immunocytochemistry analysis revealed the expression of GR in BMDCs in vehicle, DEX (10nM, 24 hours), LPS (1 ng/mL, 24 hours), or LPS+DEX treated cells. The inset shows the detailed DCs morphology. Scale bar, 10 μm. (E) FITC-dextran uptake activity was blocked by DEX in immature DCs. BMDCs were pretreated with vehicle or DEX (10nM) for 24 hours. Averages (± SD) of 4 experiments are shown (*significantly less than other treatment groups, P < .05; 1-way ANOVA followed by Tukey posthoc test). (F-G) Mature BMDCs were more sensitive to glucocorticoid killing than immature DCs. Immature and mature BMDCs were cultured and purified on a Moflo cell sorter as described in “Methods.” Sorted cells were treated with vehicle, DEX (100nM) ± RU486 (100nM) for 24 hours. Both annexinV+ (F) and dead cell (DAPI+; G) staining indicated that mature BMDCs were more sensitive to glucocorticoid killing. Averages (± SD) of 5 experiments are shown (*significantly greater than other treatment groups (annexin staining) or significantly greater than CON and RU (DAPI staining), P < .01; 1-way ANOVA followed by Tukey posthoc test).
Distinct glucocorticoid responsiveness of BMDCs. (A) Flow cytometric assessment of expression levels of CD86 and MHC II on BMDCs from control (CON), DEX (10nM, 24 hours), LPS (1 ng/mL, 24 hours), and LPS+DEX treated cultures shows that LPS induced both CD86 and MHC II, which was blocked by DEX. Experiments were repeated at least 4 times. (B) LPS (1 ng/mL, 24 hours) significantly induced TNF-α and IL-6 production by BMDCs. DEX (10nM, 24 hours) efficiently blocked the LPS-induced cytokine production. Averages (± SD) from 4 experiments are shown (*significantly greater than other treatment groups, P < .05; 1-way ANOVA followed by Tukey posthoc test). (C) T cell proliferation (CFSE) in CD4+ T cells and LPS-activated BMDC coculture was repressed when BMDCs were pretreated with DEX (10nM, 24 hours). Experiments were repeated at least 4 times. (D) Immunocytochemistry analysis revealed the expression of GR in BMDCs in vehicle, DEX (10nM, 24 hours), LPS (1 ng/mL, 24 hours), or LPS+DEX treated cells. The inset shows the detailed DCs morphology. Scale bar, 10 μm. (E) FITC-dextran uptake activity was blocked by DEX in immature DCs. BMDCs were pretreated with vehicle or DEX (10nM) for 24 hours. Averages (± SD) of 4 experiments are shown (*significantly less than other treatment groups, P < .05; 1-way ANOVA followed by Tukey posthoc test). (F-G) Mature BMDCs were more sensitive to glucocorticoid killing than immature DCs. Immature and mature BMDCs were cultured and purified on a Moflo cell sorter as described in “Methods.” Sorted cells were treated with vehicle, DEX (100nM) ± RU486 (100nM) for 24 hours. Both annexinV+ (F) and dead cell (DAPI+; G) staining indicated that mature BMDCs were more sensitive to glucocorticoid killing. Averages (± SD) of 5 experiments are shown (*significantly greater than other treatment groups (annexin staining) or significantly greater than CON and RU (DAPI staining), P < .01; 1-way ANOVA followed by Tukey posthoc test).
The ability of glucocorticoids to regulate antigen uptake appeared different between immature and mature BMDCs. DCs take up antigens via fluid-phase endocytosis (macropinocytosis), receptor-mediated endocytosis, and phagocytosis. We determined DEX regulation of FITC-dextran uptake in immature and mature BMDCs as a representative of the antigen uptake pathways. DCs take up FITC-dextran, which resembles the carbohydrate moieties of antigens from microorganisms, via receptor-dependent mechanisms and, to some degree, via macropinocytosis. FITC-dextran uptake activity was blocked by DEX (10nM, 24 hours) in control but not in LPS-treated BMDCs (Figure 4E), suggesting the glucocorticoid responsiveness of immature and mature BMDCs are different. The blockade of uptake activity of immature BMDCs was inhibited by the addition of the selective GR antagonist RU486 (10nM, 24 hours), indicating that GR mediates the inhibitory activity of DEX on the uptake activity of immature BMDCs (data not shown). Consistent with the immunocytochemistry data above, the different glucocorticoid responsiveness of the antigen uptake activity further suggests that the GR in immature and mature BMDCs may be different.
We further investigated whether BMDCs at different maturational stages have distinct sensitivity to glucocorticoid-induced apoptosis. BMDCs were matured with LPS (1 ng/mL) for 24 hours. Live immature and mature BMDCs (DAPI−CD11c+CD86−/lowMHC II−/low or DAPI−CD11c+CD86hiMHC IIhi) were sorted on a MoFlo cell sorter (DAKO). Sorted cells were cultured in the absence and presence of DEX (100nM) or corticosterone (1μM) for another 24 hours and cell viability and apoptosis were examined using flow cytometry. Sorted mature BMDCs had a higher tendency to undergo apoptosis than immature BMDCs (Figure 4F), suggesting that LPS caused apoptosis of BMDCs or mature BMDCs had more spontaneous cell death than immature BMDCs. After DEX or corticosterone treatment, mature, but not immature, BMDCs had increased apoptosis as evidenced by annexin-V staining (Figure 4F). RU486 (100nM) blocked the proapoptotic action of DEX in mature BMDCs, indicating that the glucocorticoid sensitivity of mature BMDCs is probably mediated by GR. Similar observations were obtained using a viability dye (DAPI) to detect cell death (Figure 4G). Lower concentrations of DEX (1 or 10nM) did not have significant effects on cell viability (data not shown). Therefore, in experiments where cell death confounds results, for example cytokine production and antigen uptake assays, DEX was used at 10nM. These results indicate that glucocorticoid sensitivities of immature and mature BMDCs are different and the GR in immature and mature BMDCs may be different.
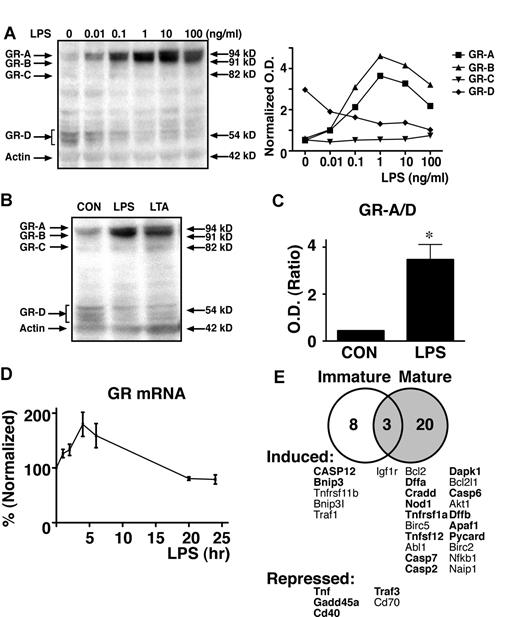
Distinct GR isoform profiles in immature and mature BMDCs
Although previous studies have examined GR expression in DCs,9,10,22,25 none of these studies have evaluated the GR translational isoforms. To determine the mechanisms underlying the maturational stage-specific glucocorticoid sensitivity of DCs, we examined the GR isoforms expressed in BMDCs at various stages of maturation using Western blot analysis. We focused on GRα isoforms because our unpublished results (N.Z.L., 2012) and others30 indicated that GRβ isoforms are undetectable in DCs. Immature BMDCs predominantly expressed the GR(α)–D isoforms whereas the predominant GR isoforms in mature BMDCs (eg, after stimulation with LPS) were the GR-A and B isoforms (Figure 5A-B). The level of the GR-C isoforms in BMDCs was negligible before and after LPS treatment. LPS dose-dependently switched the GR isoforms in BMDCs (Figure 5A). Concentrations of LPS as low as 0.01 ng/mL could induce the switch of GR isoforms in BMDCs, whereas 1 ng/mL was the optimal concentration. With 1 ng/mL of LPS, GR-A was increased approximately 6-fold, GR-B was increased approximately 8-fold; and GR-D was decreased 2-fold. Because DCs can be matured by different stimuli (Toll-like receptor (TLR) ligands, immune complexes, proinflammatory cytokines, and many others),36 we determined the GR isoform profiles in BMDCs stimulated by additional agents. We found that the TLR2 ligand, LTA (4 μg/mL, Figure 5B), switched the GR-D isoform to the GR-A isoform as effectively as LPS. The ratio of the proapoptotic GR isoforms (GR-A and B isoforms)/nonapoptotic GR-D isoforms increased from approximately 0.5 to nearly 4 after stimulation with LPS (1 ng/mL, Figure 5C). Consistent with previous findings that these GR isoforms are generated via translational mechanisms,28 GR mRNA level was found at similar levels before and after LPS treatments (Figure 5D). GR mRNA slightly increased shortly after LPS exposure and returned to baseline within 20 hours. The slight increase in GR mRNA after LPS may have contributed to the increase of the GR-A and B isoforms. In contrast, additional mechanisms probably mediated the reduced expression of the GR-D isoforms. To further determine the mechanisms underlying the distinct glucocorticoid sensitivity of immature and mature BMDCs, we performed PCR array analyses using the murine apoptosis array to compare the genes regulated by DEX (100nM, 6 hours; Figure 5E). Among 84 genes analyzed, 8 and 20 genes were uniquely regulated in immature and mature DCs, respectively. The majority of induced genes in immature DCs were antiapoptotic whereas all 3 genes repressed were proapoptotic. The majority of induced genes in mature DCs were proapoptotic, including both initiation molecules and execution enzymes. Taken together, it appears that when the GR-D isoforms are the predominant isoforms as in immature DCs, DCs are relatively resistant to glucocorticoid killing and when the proapoptotic GR isoforms, such as GR-A and B, are increased to sufficient levels as in mature DCs, apoptosis occurs after glucocorticoid exposure, probably because of the increased ratios of proapoptotic factors over antiapoptotic factors.
Distinct GR translational isoform profiles in immature and mature DCs. (A) A representative Western blot analysis shows that GR translational isoforms switched from predominantly the GR-D isoforms to GR-A and B isoforms in an LPS dose-dependent manner. Experiments were repeated at least 3 times. (B) A representative Western blot analysis shows the induction of the GR-D to GR-A isoform switch by LPS (1 ng/mL, 24 hours) and LTA (4 μg/mL, 24 hours). (C) The ratio (± SD, n = 3) of the proapoptotic GR isoforms (GR-A, B, and C isoforms) over the nonapoptotic GR-D isoforms (GR-A/GR-D) was increased significantly by LPS (1 ng/mL, 24 hours; 2-tailed t test, *P < .01). (D) Levels of GR mRNA were not significantly regulated by LPS (1 ng/mL, n = 3). Real-time RT PCR determination of mRNA levels is described in “Methods.” (E) BMDC maturational stage-specific gene regulation by DEX. BMDCs were treated with vehicle or LPS (1 ng/mL, 48 hours) before exposure to DEX (100nM, 6 hours, a time point where there was minimal cell death). The numbers of genes regulated by DEX that were revealed by the murine apoptosis PCR array analyses are indicated in the Venn diagram. Genes are listed in descending order of average fold regulation (n = 3) and proapoptotic genes are in bold.
Distinct GR translational isoform profiles in immature and mature DCs. (A) A representative Western blot analysis shows that GR translational isoforms switched from predominantly the GR-D isoforms to GR-A and B isoforms in an LPS dose-dependent manner. Experiments were repeated at least 3 times. (B) A representative Western blot analysis shows the induction of the GR-D to GR-A isoform switch by LPS (1 ng/mL, 24 hours) and LTA (4 μg/mL, 24 hours). (C) The ratio (± SD, n = 3) of the proapoptotic GR isoforms (GR-A, B, and C isoforms) over the nonapoptotic GR-D isoforms (GR-A/GR-D) was increased significantly by LPS (1 ng/mL, 24 hours; 2-tailed t test, *P < .01). (D) Levels of GR mRNA were not significantly regulated by LPS (1 ng/mL, n = 3). Real-time RT PCR determination of mRNA levels is described in “Methods.” (E) BMDC maturational stage-specific gene regulation by DEX. BMDCs were treated with vehicle or LPS (1 ng/mL, 48 hours) before exposure to DEX (100nM, 6 hours, a time point where there was minimal cell death). The numbers of genes regulated by DEX that were revealed by the murine apoptosis PCR array analyses are indicated in the Venn diagram. Genes are listed in descending order of average fold regulation (n = 3) and proapoptotic genes are in bold.
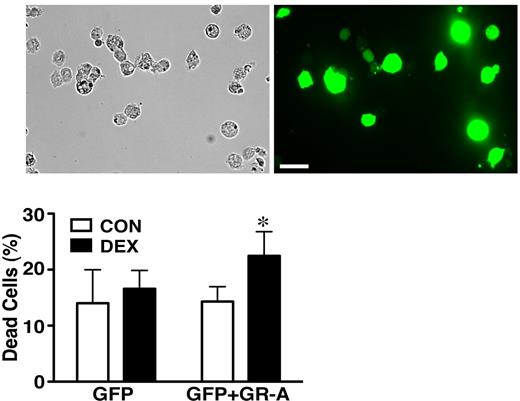
Ectopic expression of the GR-A isoform renders immature DCs sensitive to glucocorticoids
We transfected the GR-A isoform into immature BMDCs to determine whether the proapoptotic GR isoform could confer glucocorticoid sensitivity in immature BMDCs. BMDCs were transfected using Amaxa murine immature DCs transfection subroutine according to the manufacturer's protocol. Transfection efficiency was greater than 50% (Figure 6). Green fluorescent protein (GFP) or GFP+GR-A–transfected cells were purified using a MoFlo cell sorter. Isolated cells were treated with DEX (100nM) for 24 hours. Cell death was measured by propidium iodide labeling. GFP+GR positive cells, but not GFP+ cells, showed increased killing by DEX (Figure 6), indicating immature BMDCs are capable of glucocorticoid-induced cell death and the proapoptotic GR-A isoform can confer glucocorticoid sensitivity.
GR translational isoforms mediated the distinct glucocorticoid responses in immature and mature DCs. Ectopic expression of the GR-A isoform in immature BMDCs enabled glucocorticoid killing. The efficiency of Amaxa transfection of BMDCs was greater than 50%. Positively transfected cells were harvested using the Moflo cell sorter. DEX (100nM) treatment was 24 hours and dead cells were detected using propidium iodide staining (± SD, n = 3; *significantly greater than CON, P < .05; Student t test). Scale bar, 30 μm.
GR translational isoforms mediated the distinct glucocorticoid responses in immature and mature DCs. Ectopic expression of the GR-A isoform in immature BMDCs enabled glucocorticoid killing. The efficiency of Amaxa transfection of BMDCs was greater than 50%. Positively transfected cells were harvested using the Moflo cell sorter. DEX (100nM) treatment was 24 hours and dead cells were detected using propidium iodide staining (± SD, n = 3; *significantly greater than CON, P < .05; Student t test). Scale bar, 30 μm.
Human monocyte–derived DCs switch GR isoforms during maturation
To further determine the maturational stage-specific GR isoform profile of DCs, we identified GR isoforms in human monocyte–derived DCs. CD14+ cells were isolated from human peripheral blood mononuclear cells and differentiated into DCs over 7 days in culture medium containing GM-CSF and IL-4. DCs differentiation (greater then 90% purity) was confirmed by increased detection of CD1a and decreased expression of CD14. GR isoforms were determined using Western blot analysis. As in murine BMDCs, immature monocyte-derived DCs expressed predominantly the GR-D isoforms and LPS (1 ng/mL, 24 hours) induced the expression of HLA-DR molecules (not shown) and the switch from the GR-D to the GR-A isoform in human monocyte–derived DCs (Figure 7A). DEX (100nM, 48 hours) increased death in LPS-treated cells but not control cells (Figure 7B), further confirming the murine data suggesting that GR isoforms mediate the distinct glucocorticoid responsiveness of DCs at different maturational stages.
Distinct GR isoforms in human DCs. Human monocyte–derived DCs were cultured as described in “Methods.” (A) A representative Western blot analysis shows that the GR isoform switched from the GR-D (predominantly GR-D1) to the GR-A isoform after LPS (1 ng/mL, 24 hours) treatment. The ratio (± SD, n = 3) of the proapoptotic GR-A isoform over the nonapoptotic GR-D isoforms (GR-A/D) increased significantly by LPS (1 ng/mL, 24 hours; 2-tailed t test, *P < .01). (B) Representative histograms show the distinct sensitivity of control (CON) and LPS-treated cells to DEX (100nM, 48 hours). Cell death was indicated by the amount of DAPI staining. The average results (± SD, n = 4) are also shown (*significantly greater than other treatment groups, P < .05; 1-way ANOVA followed by Tukey posthoc test).
Distinct GR isoforms in human DCs. Human monocyte–derived DCs were cultured as described in “Methods.” (A) A representative Western blot analysis shows that the GR isoform switched from the GR-D (predominantly GR-D1) to the GR-A isoform after LPS (1 ng/mL, 24 hours) treatment. The ratio (± SD, n = 3) of the proapoptotic GR-A isoform over the nonapoptotic GR-D isoforms (GR-A/D) increased significantly by LPS (1 ng/mL, 24 hours; 2-tailed t test, *P < .01). (B) Representative histograms show the distinct sensitivity of control (CON) and LPS-treated cells to DEX (100nM, 48 hours). Cell death was indicated by the amount of DAPI staining. The average results (± SD, n = 4) are also shown (*significantly greater than other treatment groups, P < .05; 1-way ANOVA followed by Tukey posthoc test).
Discussion
Glucocorticoids are widely used medicines because of their anti-inflammatory and immunosuppressive activities. Glucocorticoids can suppress adaptive immune responses in part by suppressing DC maturation.7,8 We report here that glucocorticoids selectively stimulated apoptosis in mature DCs. Immature DCs, in contrast, were spared from glucocorticoid killing. Thus, our studies have uncovered a previously unknown acquisition of glucocorticoid sensitivity during DC maturation. The DC maturational stage-specific effects of glucocorticoids, depending on circulating glucocorticoid levels that are influenced by physiologic processes and pharmacologic exposure, expand the known actions of glucocorticoids on DCs: (1) suppression of the conversion of immature to mature DCs; (2) inhibition of antigen processing and presentation; (3) interference with migration of mature DCs; (4) blockade of cytokine production in mature DCs; and (5) biasing tolerogenic DCs. Because DCs serve as a liaison between innate and adaptive immunity,36 the selective sparing of immature DCs by glucocorticoids may relate to the ability of glucocorticoids to spare innate immunity.37 Sparing of immature DCs by glucocorticoids may permit the immediate innate host defense roles played by DCs. DCs at a later stage of their maturational cycle during homeostasis and inflammation, in contrast, may become susceptible to glucocorticoid-induced death. Limiting the number of mature DCs and their roles in adaptive immune response may contribute to the anti-inflammatory actions of glucocorticoids. Our finding that LPS stimulation increased the susceptibility of BMDCs to undergo glucocorticoid-induced apoptosis is in contrast to some previous reports indicating that glucocorticoids do not induce DCs apoptosis.13,16,26 The discrepancy between these studies and ours is probably because of differences in purity, types of cells, and treatment regimens. We performed apoptosis assays using immature and mature BMDCs purified using a MoFlo cell sorter and the purity of immature and mature BMDCs after sorting exceeded 97%, whereas the previous reports used unsorted BMDC cultures that contained DCs with various degrees of maturity. In some of the previous studies, immature DCs were activated with LPS for only 4 hours,16 an insufficient amount of time to synthesize new GR proteins (N.Z.L., unpublished data, 2012). DEX was used in this study and is more potent than natural glucocorticoids (eg, hydrocortisone) used in some of the previous studies. A relatively high dose of DEX (equal to or greater than 100nM) is required to kill mature DCs. However, our findings do agree with the majority of the literature that demonstrates that DCs are sensitive to glucocorticoid killing.7,9,10,12,15,18-25 The maturational stage-specific sensitivity of DCs to glucocorticoid-induced apoptosis is thus a novel mechanism underlying the anti-inflammatory and immunosuppressive activities of glucocorticoids.
This is the first study that identifies the GR translational isoforms in DCs. The GR-A and B isoforms in mature BMDCs were efficient in mediating glucocorticoid killing. In addition, the GR-D isoforms in immature DCs were functional as demonstrated by their ability to inhibit the expression of CD86 and MHC II (Figure 4A DEX versus CON), suppress antigen uptake (Figure 4E) and regulate gene expression (Figure 5E). Similar to observations made previously in various cell lines and tissues,28 multiple GR isoforms coexist in DCs. Increasing the amount of the GR-D isoforms does not inhibit the activity of the proapoptotic GR isoforms,28,38 suggesting that GR-D isoforms do not have dominant negative activities. Rather, the GR-D isoforms probably contribute to altering glucocorticoid responses via regulating GR-D isoform-specific target genes. Cell type-specific actions of glucocorticoids contribute to their anti-inflammatory effects. Glucocorticoids are proapoptotic in various immune cells, including T cells, monocytes/macrophages, osteoblasts, eosinophils, basophils, and DCs. Glucocorticoids are antiapoptotic in cells involved in barrier function and tissue repair, such as fibroblasts and specific epithelia. It will be worthwhile to determine the GR isoforms in additional immune cells as well as non-immune cells to understand cell-specific actions of glucocorticoids. Such information may identify strategies to enhance the anti-inflammatory effects of glucocorticoids while reducing their side effects. Specific targeting of the GR-D isoforms in immature DCs might be expected to maintain host defense and suppress inflammation. Previously we found that the GR-D isoforms, unlike the other GR-isoforms, do not trigger apoptosis of an osteoblast cell line.31 Therefore a potential strategy to avoid osteoporosis, a major side effect of glucocorticoids, may be to selectively target the GR-D isoform.
The GR-D to GR-A isoform switch during DC maturation appeared to be regulated at the translational level because GR mRNA level was only marginally and transiently increased after LPS stimulation. We previously described that translational mechanisms including ribosomal leak scanning and ribosomal shunting are responsible for the generation of GR isoforms. All GR translational isoforms have similar turnover rates28 because all GR isoforms have the same PEST domain that serves as the interaction domain between GR and proteasomes.39 It has been reported that mRNA-specific structures regulate alternative translation of heat shock protein 70 and several viral genes.40,41 However, similar structures in GR mRNA have not been identified. The components of the translation machinery are numerous and it is probable that multiple translation factors work in a coordinated fashion to regulate GR translation. LPS and other inflammatory signals that switch GR isoforms probably do so via effects on these translational mechanisms. The mechanisms underlying the translational regulation of GR isoforms could potentially provide new strategies to alter or enhance the cellular expression of GR isoforms and glucocorticoid responses.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the personnel at the Robert H. Lurie Comprehensive Cancer Center flow cytometry facility for assistance with cell sorting.
This work was supported by National Institutes of Health grants NIH 1R01HL094558-01A1 (N.Z.L.) NIH 3R01HL094558-01A1S1 (N.Z.L.), and NIH 2R37HL068546-26 (R.P.S).
National Institutes of Health
Authorship
Contribution: N.Z.L. and R.P.S. designed the research; Y.C., I.K.B., A.K.K., S.C.S., and N.Z.L. performed the research; Y.C., N.Z.L., J.A.C., and R.P.S. analyzed and discussed the data; N.Z.L. and R.P.S. wrote the paper; and C.M.J. provided technical assistance.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for A.K.K. is University of Ioannina Medical School, Ioannina, Greece.
Correspondence: Nick Z. Lu, Division of Allergy-Immunology, Dept of Medicine, Feinberg School of Medicine, Northwestern University, McGaw Rm M301, 240 E Huron, Chicago, IL 60611; e-mail: nickzlu@northwestern.edu.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal