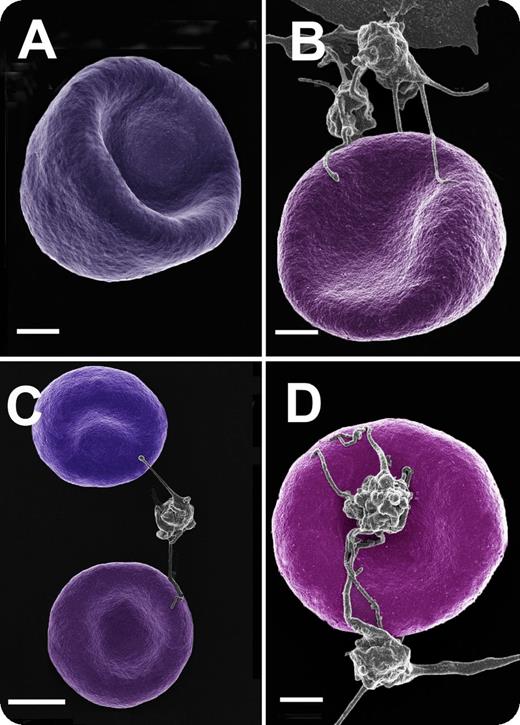
Throughout a healthy pregnancy, there is a general elevation of hemostatic activation markers, and research has shown that platelet activation contributes to a general hypercoagulable state. Here, we studied healthy individuals during early and late pregnancy and also postpartum. There were 30 females per group, and they did not smoke or take any medication before or during their pregnancy. Red blood cell (RBC) and platelet ultrastructure were studied using blood smears and scanning electron microscopy to determine if there is a changed ultrastructure during a healthy pregnancy. Blood smears show a typical RBC from a female of childbearing age, typically with no platelet association (panel A, bar represents 1 μm), and RBCs during early and late pregnancy, as well as 6 to 8 weeks postpartum (panels B-D, respectively; bars represent 1 μm). During these 3 stages, almost all RBCs in the whole blood smears were closely associated with platelets, showing platelet spreading and pseudopodia closely associated with RBC membranes. Although, in all samples, 1 RBC is typically involved with only 1 platelet, we have noted that a single platelet may have multiple interactions with RBCs (panel C).
Here we suggest that these interactions between RBCs and platelets may be one of the reasons for an increased hypercoagulability during a healthy pregnancy, and this state continues for a while postpartum. Thus, these RBC/platelet interactions could possibly contribute to gestational thrombocytopenia.
Throughout a healthy pregnancy, there is a general elevation of hemostatic activation markers, and research has shown that platelet activation contributes to a general hypercoagulable state. Here, we studied healthy individuals during early and late pregnancy and also postpartum. There were 30 females per group, and they did not smoke or take any medication before or during their pregnancy. Red blood cell (RBC) and platelet ultrastructure were studied using blood smears and scanning electron microscopy to determine if there is a changed ultrastructure during a healthy pregnancy. Blood smears show a typical RBC from a female of childbearing age, typically with no platelet association (panel A, bar represents 1 μm), and RBCs during early and late pregnancy, as well as 6 to 8 weeks postpartum (panels B-D, respectively; bars represent 1 μm). During these 3 stages, almost all RBCs in the whole blood smears were closely associated with platelets, showing platelet spreading and pseudopodia closely associated with RBC membranes. Although, in all samples, 1 RBC is typically involved with only 1 platelet, we have noted that a single platelet may have multiple interactions with RBCs (panel C).
Here we suggest that these interactions between RBCs and platelets may be one of the reasons for an increased hypercoagulability during a healthy pregnancy, and this state continues for a while postpartum. Thus, these RBC/platelet interactions could possibly contribute to gestational thrombocytopenia.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal