In this issue of Blood, 2 independent studies analyzed the relevance of the von Willebrand factor (VWF)–ADAMTS13 axis in a murine model of myocardial ischemia/reperfusion injury. It is demonstrated that genetic ablation, neutralization or increased cleavage of VWF is protective in this experimental setting.1,2 This strongly supports the concept that interference with the ADAMTS13-VWF axis may be a powerful approach to treat acute thrombo-inflammatory disease states.
Von Willebrand factor (VWF) is a large multimeric protein that is stored as ultra-large von Willebrand factor (UL-VWF) in Weibel-Palade bodies of endothelial cells and in platelet α-granules from where it is released in response to injury or inflammation. Under high shear stress, VWF immobilized on exposed subendothelial collagen or on the surface of activated endothelial cells exposes its binding sites for the platelet receptor glycoprotein (GP) Ib. GPIb-VWF interactions mediate platelet deceleration, thereby allowing other receptors to interact with their ligands to induce cellular activation, firm adhesion, and thrombus formation. This process is crucial to limit posttraumatic blood loss, but also causes myocardial infarction and ischemic stroke, the 2 leading causes of death and severe disability worldwide.
UL-VWF is the most thrombogenic VWF variant and its activity is tightly controlled by the plasma metalloprotease ADAMTS13 that rapidly cleaves it into smaller and less thrombogenic VWF multimers, which circulate in the plasma. This process is essential to prevent excessive intravascular thrombus formation as revealed in patients who suffer from thrombotic thrombocytopenic purpura (TTP), a severe thrombotic disease state caused by acquired ADAMTS13-inhibiting autoantibodies or genetic defects resulting in reduced ADAMTS13 activity.3 Likewise, increased levels of VWF or decreased levels of ADAMTS13 are associated with an increased risk of ischemic stroke and myocardial infarction.4 Animal studies have shown that the balance of the VWF-ADAMTS13 axis is a critical determinant of cerebral ischemia/reperfusion injury because absence of VWF5 or increased levels of ADAMTS136 are beneficial, while ADAMTS13 deficiency has detrimental effects on infarct size and neurologic outcome after focal cerebral ischemia.6,7 Unexpectedly, however, this pathology appears to occur independently of platelet aggregation as anti-GPIIb/IIIa antibodies were not protective in this setting in mice and humans.8 These data in combination with the observation that cerebral ischemia also elicits a strong inflammatory response with an essential but not fully understood critical involvement of T cells9,10 led to the concept of thrombo-inflammation as a principal pathomechanism of ischemic stroke.8 A crucial role of VWF within this concept is further supported by a recent study of Petri et al demonstrating that VWF (and also GPIb) is crucial for efficient leukocyte extravasation during inflammation.11
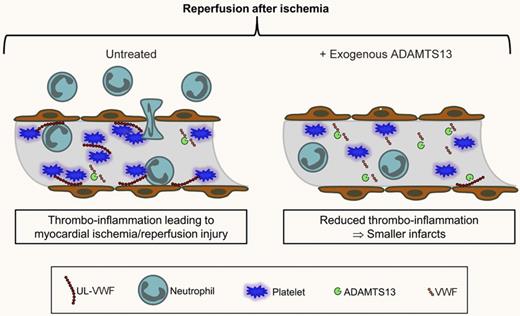
The 2 studies published in this issue of Blood now expand the importance of the VWF-ADAMTS13 axis to acute myocardial infarction. In a murine model of cardiac ischemia/reperfusion injury they show that ADAMTS13 deficiency resulted in increased infarct sizes while absence or antibody-blockade of VWF2 as well as the pre-treatment with recombinant human (rh) ADAMTS131 reduced infarct sizes, and consequently, cardiomyocyte apoptosis. Interestingly, this protective effect was associated with reduced neutrophil infiltration into the ischemic myocardium, indicating that VWF activity also determines leukocyte recruitment in cardiac ischemia/reperfusion injury (see figure).1,2 This suggests that ischemia/reperfusion injury in the brain and in the heart might both be thrombo-inflammatory processes, implying that the pathomechanisms of the 2 leading causes of death might be more similar than previously thought. In the light of the results of De Meyer et al who infused rhADAMTS13 into mice1 one might speculate that only the UL-VWF (but not the smaller, cleaved VWF multimers) contribute to the pathology of ischemia/reperfusion injury. However, further studies will be required to confirm this hypothesis. Of note VWF neutralizing antibodies2 as well as rhADAMTS131 were infused in parallel with the onset of ischemia that may not exactly reflect the situation in patients with acute myocardial infarction. Therefore, it will be important to test the efficacy of rhADAMTS13 treatment at later time points during the reperfusion phase. Assuming that these studies will also support the therapeutic use of rhADAMTS13, or similar strategies, modulation of VWF activity appears to be an attractive therapeutic approach to treat myocardial infarction as well as acute ischemic stroke. We hope that this will encourage preclinical studies to translate this promising approach from animals to patients.
ADAMTS13-mediated modulation of VWF activity limits thrombo-inflammatory ischemia/reperfusion injury in the heart. In the ischemic heart, ultra-large (UL)–VWF released from activated or damaged endothelial cells and platelets promotes neutrophil and platelet recruitment that contribute to tissue damage. UL-VWF is cleaved by ADAMTS13 to smaller VWF multimers that circulate in the plasma and are less potent in recruiting neutrophils and platelets. Infusion of exogenous ADAMTS13 reduces UL-VWF levels and infarct size. Similar results were obtained in VWF-deficient mice or mice treated with anti-VWF antibodies. The exact mechanism of how VWF, platelets, and leukocytes promote these processes to induce tissue damage remains to be determined.
ADAMTS13-mediated modulation of VWF activity limits thrombo-inflammatory ischemia/reperfusion injury in the heart. In the ischemic heart, ultra-large (UL)–VWF released from activated or damaged endothelial cells and platelets promotes neutrophil and platelet recruitment that contribute to tissue damage. UL-VWF is cleaved by ADAMTS13 to smaller VWF multimers that circulate in the plasma and are less potent in recruiting neutrophils and platelets. Infusion of exogenous ADAMTS13 reduces UL-VWF levels and infarct size. Similar results were obtained in VWF-deficient mice or mice treated with anti-VWF antibodies. The exact mechanism of how VWF, platelets, and leukocytes promote these processes to induce tissue damage remains to be determined.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal