Abstract
Abstract  921
921
This 3+3 dose escalation phase I trial by the German MDS study group aimed to determine the dose-limiting toxicity (DLT) and maximum tolerated dose (MTD) of sequential azacitidine (AZA) 75 mg/m2 for 5 days followed by 14 days of up to 25 mg lenalidomide (LEN) in patients with higher-risk myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) and del(5q) cytogenetic abnormalities. Twenty patients (median age 69 years) were enrolled, including 16 (80%) with complex cytogenetic abnormalities and 65% of patients harboring at least one TP53 mutation. Nine patients (45%) had no prior treatment while relapse or progression to single agent azacitidine or lenalidomide treatment (30%) and allogeneic HSCT (15%) were the most common regimens among previously treated patients.
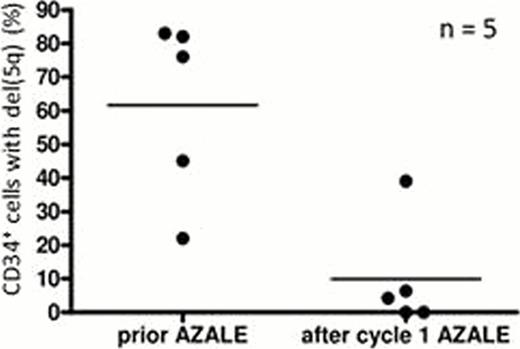
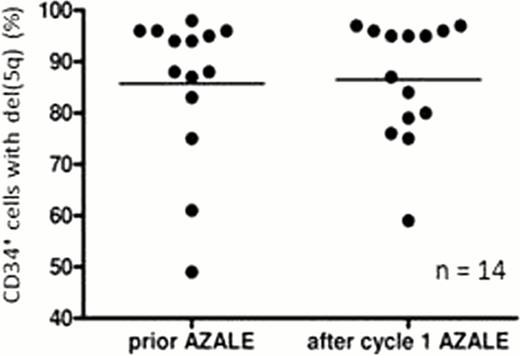
Three of 6 patients treated with LEN at the 25 mg dose level experienced DLTs, with 20 mg subsequently identified as MTD. All eligible patients experienced treatment-related Grade 3/4 thrombocytopenia and neutropenia. Hematologic responses occurred in 4 of 9 (44%) previously untreated patients with complex karyotypes, including 3 with a TP53 mutation and were preceded by a significant decrease of del(5q) CD34+ progenitor cells in the blood during cycle 1. In fact, compared with baseline, the percentage of peripheral blood CD34+ cells with del(5q) clone was decreased in the hematologic responders after 1 cycle of azacitidine followed by lenalidomide therapy (P = 0.001) (Figure 1A). In contrast, the percentage of peripheral blood CD34+ cells with del(5q) remained unchanged in hematologic non-responders (Figure 1B). By applying TP53 mutation directed deep-sequencing technology we observed a concomitant early reduction and disappearance of minimal residual disease in MDS patients achieving a complete cytogenetic response. In one patient, a reemergence of the TP53 clone was observed later despite continuation of the treatment but by consolidation (lower dose and every 8 weeks compared to 4 weeks with induction) and it preceded the hematologic and cytogenetic relapse by several months.
In conclusion, in a population of higher-risk MDS/AML patients with del(5q) that included a high proportion of patients with complex karyotypes and mutations of TP53, the sequential combination of azacitidine and lenalidomide was shown to be a feasible and potentially effective treatment strategy, even in those patients with TP53 -mutated clones. We additionally observed a correlation between the percentage of peripheral CD34+ cells with del(5q) and hematologic response, suggesting that monitoring of this cell population may be a surrogate marker of response in this setting. Our results encourage an application of sequential azacitidine and lenalidomide as first line therapy for higher-risk MDS patients in future trials.
(A) HEMATOLOGIC RESPONDERS (B) HEMATOLOGIC NON-RESPONDERS
(A) HEMATOLOGIC RESPONDERS (B) HEMATOLOGIC NON-RESPONDERS
Platzbecker:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Kuendgen:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees. Götze:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees. Giagounidis:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees. Germing:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees. Haase:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal