Abstract
Abstract 891
The Transforming growth factor β (TGF-β) signaling pathway has been previously known to play a tumor suppressor role in hematologic malignancies. Smad proteins and their phosphorylation play a vital role in TGF-β signaling pathway. There are three class of Smads; Receptor-regulated Smads (1, 2, 3, 5, 8), Common mediator Smad (4) and Inhibitory Smads (6, 7). However, little is known about the expression and activation of Smad proteins in AML and nothing has been reported about correlation with clinical features or outcomes. Interestingly, Tabe et.al, (ASH 2012) recently identified pro-survival effect of TGF-β in leukemia cells via upregulation of MMP-1 and that the anti-apoptotic effect of TGF-β was associated with G0/G1 cell cycle arrest
We performed proteomic profiling of Smad expression, measuring the level of total Smad 1, 2, 3, 4, 5, 6, and phosphorylated Smad 2 (p245, p465) and 5 (p463) using reverse phase protein array (RPPA) technology. All antibodies were strictly validated. Analysis was performed on a cohort of 511 newly diagnosed AML (non APL) cases randomly divided into training and test sets. Normal bone marrow derived CD34+ cells (n=11) served as expression controls. Hierarchical clustering with Wald linkage rules and Euclidean distance matrix were used to define signatures. Cox model and long rank test were used to assess the survival outcome with different sample signatures.
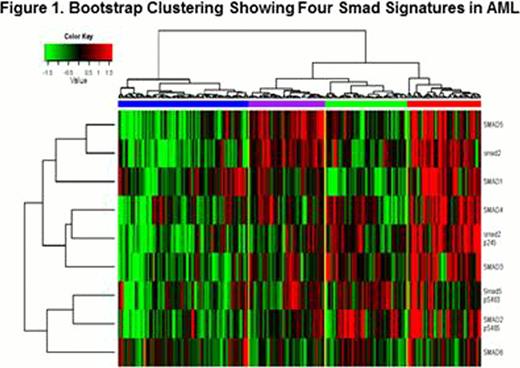
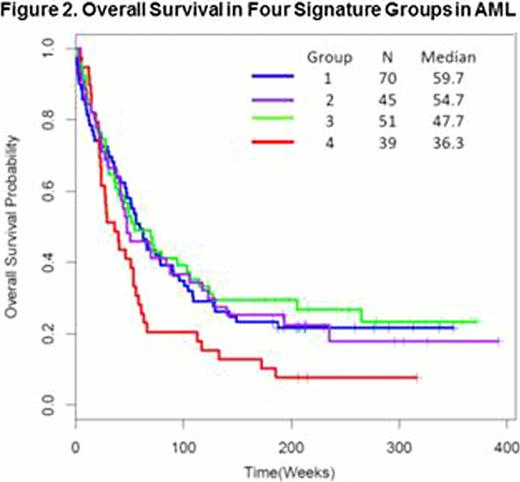
When comparing expression of individual Smad proteins with control CD34+ cells, most cases had expression within the normal CD34+ cell range, but levels of Smad 2, 2p465 and 4 had higher percentages of cases with expression below normal, while levels of Smad 3, 5, 5 (p463) and 6 were more frequently expressed at levels above normal. There were no major differences in expression between bone marrow and blood, and diagnosis and relapse samples. When unbiased hierarchical clustering was performed on the training set, four distinct Smad protein expression signatures were identified (Figure 1). Group 1 is characterized by pan-low Smad expression; Group 2 by high expression in Smad 2, 5, 5 (p463); Group 3 by high expression of phosphorylated Smad 2 (p245, p465) and 5 (p463); and Group 4, by pan-high Smad expression. Group 2 was associated with Ras mutation (28% vs. 9% for the other 3, p=0.03) and FLT3 ITD (p=0.009) mutation frequency was significantly lower in group 1. Smad group was not associated with FAB classification, demographics, prior treatment history, cytogenetics, and other molecular mutations. Higher Smad expression was statistically significantly correlated with higher counts of WBC (p=0.04), bone marrow and peripheral blast % (p=0.009, 0.004), CD33 and 34 counts (p=0.006, 0.002). Intriguingly, among 210 other proteins assayed in RPPA, expression of Integrin/Adhesion proteins IGFBP2, CD49B, CD11A and Fibronectin were inversely correlated with Smad expression consistent with the above observation. Pan Smad expression was strongly correlated with AKT pathway activation and high expression of several proliferation promoting proteins. Pan-high Smad expression (group 4) was associated with inferior overall survival (OS) (Figure 2) and event free survival (EFS) whereas the OS and EFS of Group 1, 2, and 3 were similar (log-rank test OS p=0.017; EFS p=0.03). Median OS, EFS were 36.3 and 19.3 weeks in Group 4 versus 56.1 and 26.9 weeks in other groups, respectively. Patients in group 4 had a lower remission rate (51% vs. 66%). When validated with the test set, similar results were observed and group 4 again had inferior survival (median 26.7 vs. 58 weeks, p = 0.0047) compared to the other groups.
In conclusion, we observed that Smad expression in AML segregates into four distinct heterogeneous expression and activation patterns. Pan-high Smad expression was linked with significantly worse OS, EFS, and trends for inferior CR rates. The clinical features (high WBC and % PB and BM blasts) and inferior clinical outcome associated with pan-high Smad expression suggest that dominant TGF-β signaling is adverse in AML and that these patients may benefit from TGF-β blockade. Our finding suggest a tumor promoting, rather than tumor suppressing role, for TGF- β in AML, possibly mediated via MMP-1 activation. Further studies are required to investigate the mechanism of TGF-β pathway activation possibly inducing chemotherapy resistance leading to poor survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal